1. Kaufmann CN, Eyler LT. The role of sleep in accelerated cognitive aging in bipolar disorder. Chronobiol Med 2019;1:66ŌĆō68.

2. Turek FW. Circadian clocks: not your grandfatherŌĆÖs clock. Science 2016;354:992ŌĆō993.


5. Reppert SM, Weaver DR. Coordination of circadian timing in mammals. Nature 2002;418:935ŌĆō941.


6. Meijer JH, Michel S. Neurophysiological analysis of the suprachiasmatic nucleus: a challenge at multiple levels. Methods Enzymol 2015;552:75ŌĆō102.

7. Moore RY, Eichler VB. Loss of a circadian adrenal corticosterone rhythm following suprachiasmatic lesions in the rat. Brain Res 1972;42:201ŌĆō206.


8. Richter CP. Inborn nature of the ratŌĆÖs 24-hour clock. J Comp Physiol Psychol 1971;75:1ŌĆō4.


10. Turek FW. Circadian neural rhythms in mammals. Annu Rev Physiol 1985;47:49ŌĆō64.


11. Ralph MR, Foster RG, Davis FC, Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Science 1990;247:975ŌĆō978.


12. Welsh DK, Logothetis DE, Meister M, Reppert SM. Individual neurons dissociated from rat suprachiasmatic nucleus express independently phased circadian firing rhythms. Neuron 1995;14:697ŌĆō706.


13. Cermakian N, Sassone-Corsi P. Multilevel regulation of the circadian clock. Nat Rev Mol Cell Biol 2000;1:59ŌĆō67.


14. King DP, Takahashi JS. Molecular genetics of circadian rhythms in mammals. Annu Rev Neurosci 2000;23:713ŌĆō742.


15. Shearman LP, Zylka MJ, Weaver DR, Kolakowski LF Jr, Reppert SM. Two period homologs: circadian expression and photic regulation in the suprachiasmatic nuclei. Neuron 1997;19:1261ŌĆō1269.


18. Balsalobre A, Damiola F, Schibler U. A serum shock induces circadian gene expression in mammalian tissue culture cells. Cell 1998;93:929ŌĆō937.


20. Bargiello TA, Jackson FR, Young MW. Restoration of circadian behavioural rhythms by gene transfer in Drosophila. Nature 1984;312:752ŌĆō754.


21. Reddy P, Zehring WA, Wheeler DA, Pirrotta V, Hadfield C, Hall JC, et al. Molecular analysis of the period locus in Drosophila melanogaster and identification of a transcript involved in biological rhythms. Cell 1984;38:701ŌĆō710.


22. Panda S, Hogenesch JB, Kay SA. Circadian rhythms from flies to human. Nature 2002;417:329ŌĆō335.


23. Gallego M, Virshup DM. Post-translational modifications regulate the ticking of the circadian clock. Nat Rev Mol Cell Biol 2007;8:139ŌĆō148.


26. Jeong J, Lee Y, Cho CH, Lee HJ. Circadian gene variations are associated with obsessive-compulsive behaviors in a young healthy Korean population. Chronobiol Med 2019;1:115ŌĆō120.

27. Folkard S, Wever RA, Wildgruber CM. Multi-oscillatory control of circadian rhythms in human performance. Nature 1983;305:223ŌĆō226.


28. Monk TH, Weitzman ED, Fookson JE, Moline ML, Kronauer RE, Gander PH. Task variables determine which biological clock controls circadian rhythms in human performance. Nature 1983;304:543ŌĆō545.


29. Monk TH, Weitzman ED, Fookson JE, Moline ML. Circadian rhythms in human performance efficiency under free-running conditions. Chronobiologia 1984;11:343ŌĆō354.

30. Davies JA, Navaratnam V, Redfern PH. A 24-hour rhythm in passive-avoidance behaviour in rats. Psychopharmacologia 1973;32:211ŌĆō214.


31. Holloway FA, Wansley RA. Multiple retention deficits at periodic intervals after active and passive avoidance learning. Behav Biol 1973;9:1ŌĆō14.


32. Tapp WN, Holloway FA. Phase shifting circadian rhythms produces retrograde amnesia. Science 1981;211:1056ŌĆō1058.


33. Fekete M, van Ree JM, Niesink RJ, de Wied D. Disrupting circadian rhythms in rats induces retrograde amnesia. Physiol Behav 1985;34:883ŌĆō887.


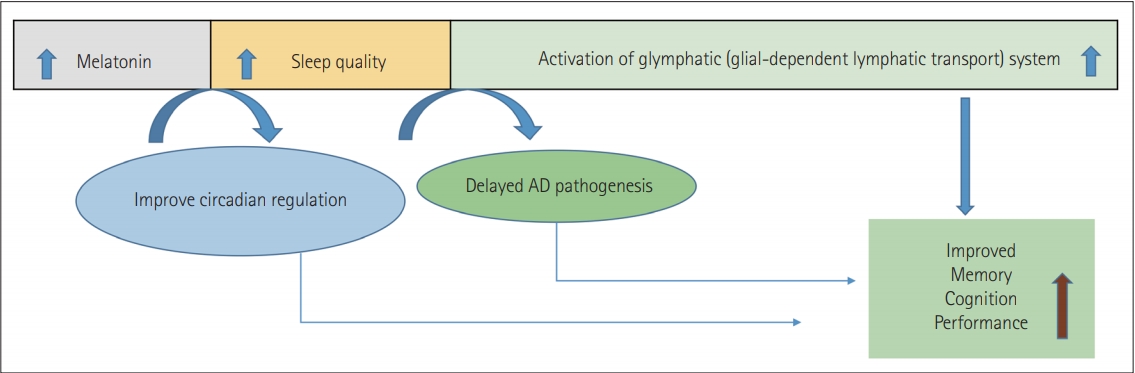
36. Fu W, Xie H, Laudon M, Zhou S, Tian S, You Y. Piromelatine ameliorates memory deficits associated with chronic mild stress-induced anhedonia in rats. Psychopharmacology (Berl) 2016;233:2229ŌĆō2239.


37. Sharif R, Aghsami M, Gharghabi M, Sanati M, Khorshidahmad T, Vakilzadeh G, et al. Melatonin reverses H-89 induced spatial memory deficit: involvement of oxidative stress and mitochondrial function. Behav Brain Res 2017;316:115ŌĆō124.


38. McArthur AJ, Gillette MU, Prosser RA. Melatonin directly resets the rat suprachiasmatic circadian clock in vitro. Brain Res 1991;565:158ŌĆō161.


39. Rusak B, Yu GD. Regulation of melatonin-sensitivity and firing-rate rhythms of hamster suprachiasmatic nucleus neurons: pinealectomy effects. Brain Res 1993;602:200ŌĆō204.


40. Starkey SJ, Walker MP, Beresford IJ, Hagan RM. Modulation of the rat suprachiasmatic circadian clock by melatonin in vitro. Neuroreport 1995;6:1947ŌĆō1951.


41. Musshoff U, Riewenherm D, Berger E, Fauteck JD, Speckmann EJ. Melatonin receptors in rat hippocampus: molecular and functional investigations. Hippocampus 2002;12:165ŌĆō173.


42. Benloucif S, Guico MJ, Reid KJ, Wolfe LF, LŌĆÖhermite-Bal├®riaux M, Zee PC. Stability of melatonin and temperature as circadian phase markers and their relation to sleep times in humans. J Biol Rhythms 2005;20:178ŌĆō188.


43. Cahill GM. Circadian regulation of melatonin production in cultured zebrafish pineal and retina. Brain Res 1996;708:177ŌĆō181.


44. Abran D, Anctil M, Ali MA. Melatonin activity rhythms in eyes and cerebral ganglia of Aplysia californica. Gen Comp Endocrinol 1994;96:215ŌĆō222.


45. Goto M, Oshima I, Tomita T, Ebihara S. Melatonin content of the pineal gland in different mouse strains. J Pineal Res 1989;7:195ŌĆō204.


47. Pandi-Perumal SR, Srinivasan V, Maestroni GJ, Cardinali DP, Poeggeler B, Hardeland R. Melatonin: natureŌĆÖs most versatile biological signal? FEBS J 2006;273:2813ŌĆō2838.

49. Hardeland R, Cardinali DP, Brown GM, Pandi-Perumal SR. Melatonin and brain inflammaging. Prog Neurobiol 2015;127-128:46ŌĆō63.


50. Manchester LC, Coto-Montes A, Boga JA, Andersen LP, Zhou Z, Galano A, et al. Melatonin: an ancient molecule that makes oxygen metabolically tolerable. J Pineal Res 2015;59:403ŌĆō419.


51. Moretti R, Zanin A, Pansiot J, Spiri D, Manganozzi L, Kratzer I, et al. Melatonin reduces excitotoxic blood-brain barrier breakdown in neonatal rats. Neuroscience 2015;311:382ŌĆō397.


52. Rudnitskaya EA, Muraleva NA, Maksimova KY, Kiseleva E, Kolosova NG, Stefanova NA. Melatonin attenuates memory impairment, amyloid-╬▓ accumulation, and neurodegeneration in a rat model of sporadic AlzheimerŌĆÖs disease. J Alzheimers Dis 2015;47:103ŌĆō116.


56. Morgan PJ, Barrett P, Howell HE, Helliwell R. Melatonin receptors: localization, molecular pharmacology and physiological significance. Neurochem Int 1994;24:101ŌĆō146.


57. Bertaina-Anglade V, Drieu-La-Rochelle C, Moca├½r E, Seguin L. Memory facilitating effects of agomelatine in the novel object recognition memory paradigm in the rat. Pharmacol Biochem Behav 2011;98:511ŌĆō517.


58. He P, Ouyang X, Zhou S, Yin W, Tang C, Laudon M, et al. A novel melatonin agonist Neu-P11 facilitates memory performance and improves cognitive impairment in a rat model of AlzheimerŌĆÖ disease. Horm Behav 2013;64:1ŌĆō7.


59. Argyriou A, Prast H, Philippu A. Melatonin facilitates short-term memory. Eur J Pharmacol 1998;349:159ŌĆō162.


61. Pandi-Perumal SR, BaHammam AS, Brown GM, Spence DW, Bharti VK, Kaur C, et al. Melatonin antioxidative defense: therapeutical implications for aging and neurodegenerative processes. Neurotox Res 2013;23:267ŌĆō300.


62. Furio AM, Brusco LI, Cardinali DP. Possible therapeutic value of melatonin in mild cognitive impairment: a retrospective study. J Pineal Res 2007;43:404ŌĆō409.


63. Esteban S, Nicolaus C, Garmundi A, Rial RV, Rodr├Łguez AB, Ortega E, et al. Effect of orally administered L-tryptophan on serotonin, melatonin, and the innate immune response in the rat. Mol Cell Biochem 2004;267:39ŌĆō46.


64. Rosales-Corral SA, Acu├▒a-Castroviejo D, Coto-Montes A, Boga JA, Manchester LC, Fuentes-Broto L, et al. AlzheimerŌĆÖs disease: pathological mechanisms and the beneficial role of melatonin. J Pineal Res 2012;52:167ŌĆō202.


65. Khan ZA, Hong Y, Choi J, Lee Y, Jin Y, Hong Y. Melatonin: a potent therapeutic candidate in degenerative neural damages. Chronobiol Med 2020;2:85ŌĆō95.

66. Mukda S, Panmanee J, Boontem P, Govitrapong P. Melatonin administration reverses the alteration of amyloid precursor protein-cleaving secretases expression in aged mouse hippocampus. Neurosci Lett 2016;621:39ŌĆō46.


67. Rudnitskaya EA, Maksimova KY, Muraleva NA, Logvinov SV, Yanshole LV, Kolosova NG, et al. Beneficial effects of melatonin in a rat model of sporadic AlzheimerŌĆÖs disease. Biogerontology 2015;16:303ŌĆō316.


68. Cardinali DP, Vigo DE, Olivar N, Vidal MF, Furio AM, Brusco LI. Therapeutic application of melatonin in mild cognitive impairment. Am J Neurodegener Dis 2012;1:280ŌĆō291.


70. Lee CH, Yoo KY, Choi JH, Park OK, Hwang IK, Kwon YG, et al. MelatoninŌĆÖs protective action against ischemic neuronal damage is associated with up-regulation of the MT2 melatonin receptor. J Neurosci Res 2010;88:2630ŌĆō2640.


71. Lee EJ, Lee MY, Chen HY, Hsu YS, Wu TS, Chen ST, et al. Melatonin attenuates gray and white matter damage in a mouse model of transient focal cerebral ischemia. J Pineal Res 2005;38:42ŌĆō52.


72. Letechip├Ła-Vallejo G, L├│pez-Loeza E, Espinoza-Gonz├Īlez V, Gonz├Īlez-Burgos I, Olvera-Cort├®s ME, Moral├Ł G, et al. Long-term morphological and functional evaluation of the neuroprotective effects of post-ischemic treatment with melatonin in rats. J Pineal Res 2007;42:138ŌĆō146.


73. Lee MY, Kuan YH, Chen HY, Chen TY, Chen ST, Huang CC, et al. Intravenous administration of melatonin reduces the intracerebral cellular inflammatory response following transient focal cerebral ischemia in rats. J Pineal Res 2007;42:297ŌĆō309.


74. Tyagi E, Agrawal R, Nath C, Shukla R. Effect of melatonin on neuroinflammation and acetylcholinesterase activity induced by LPS in rat brain. Eur J Pharmacol 2010;640:206ŌĆō210.


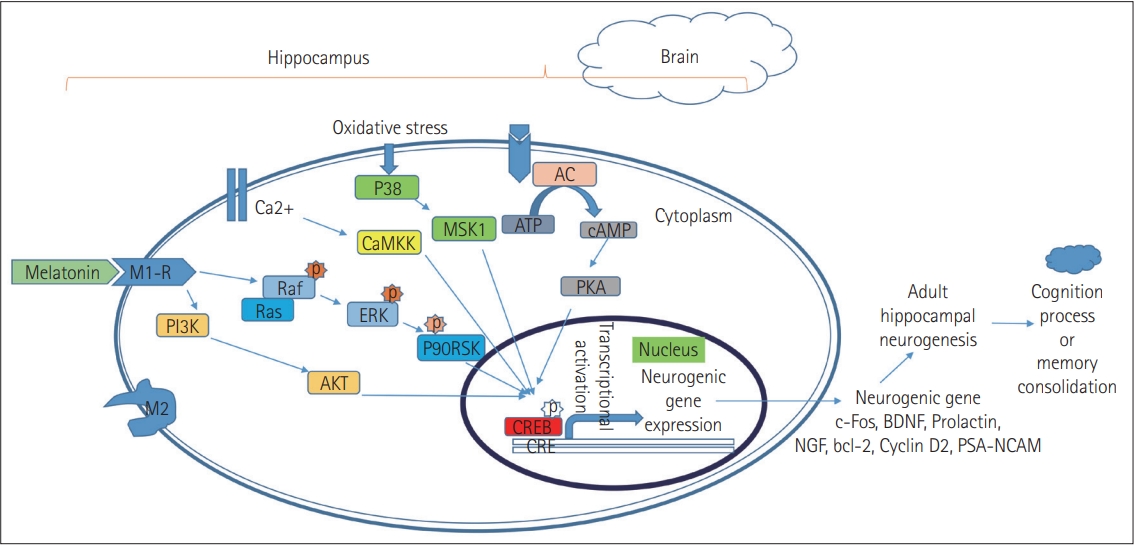
76. Kudo K, Wati H, Qiao C, Arita J, Kanba S. Age-related disturbance of memory and CREB phosphorylation in CA1 area of hippocampus of rats. Brain Res 2005;1054:30ŌĆō37.


77. Hardeland R. Melatonin and the theories of aging: a critical appraisal of melatoninŌĆÖs role in antiaging mechanisms. J Pineal Res 2013;55:325ŌĆō356.


78. Schmid HA. Decreased melatonin biosynthesis, calcium flux, pineal gland calcification and aging: a hypothetical framework. Gerontology 1993;39:189ŌĆō199.


79. Reiter RJ. The pineal gland and melatonin in relation to aging: a summary of the theories and of the data. Exp Gerontol 1995;30:199ŌĆō212.


80. Zhang HM, Zhang Y. Melatonin: a well-documented antioxidant with conditional pro-oxidant actions. J Pineal Res 2014;57:131ŌĆō146.


81. Bekinschtein P, Cammarota M, Igaz LM, Bevilaqua LR, Izquierdo I, Medina JH. Persistence of long-term memory storage requires a late protein synthesis- and BDNF- dependent phase in the hippocampus. Neuron 2007;53:261ŌĆō277.


82. Cui P, Yu M, Luo Z, Dai M, Han J, Xiu R, et al. Intracellular signaling pathways involved in cell growth inhibition of human umbilical vein endothelial cells by melatonin. J Pineal Res 2008;44:107ŌĆō114.


83. Reiter RJ. The ageing pineal gland and its physiological consequences. Bioessays 1992;14:169ŌĆō175.


84. Corrales A, Mart├Łnez P, Garc├Ła S, Vidal V, Garc├Ła E, Fl├│rez J, et al. Longterm oral administration of melatonin improves spatial learning and memory and protects against cholinergic degeneration in middle-aged Ts65Dn mice, a model of Down syndrome. J Pineal Res 2013;54:346ŌĆō358.


85. Cheng S, Ma C, Qu H, Fan W, Pang J, He H. Differential effects of melatonin on hippocampal neurodegeneration in different aged accelerated senescence prone mouse-8. Neuro Endocrinol Lett 2008;29:91ŌĆō99.

86. Yoo DY, Kim W, Lee CH, Shin BN, Nam SM, Choi JH, et al. Melatonin improves D-galactose-induced aging effects on behavior, neurogenesis, and lipid peroxidation in the mouse dentate gyrus via increasing pCREB expression. J Pineal Res 2012;52:21ŌĆō28.


87. Ali T, Badshah H, Kim TH, Kim MO. Melatonin attenuates D-galactoseinduced memory impairment, neuroinflammation and neurodegeneration via RAGE/NF-K B/JNK signaling pathway in aging mouse model. J Pineal Res 2015;58:71ŌĆō85.


88. Flood JF, Morley JE. Learning and memory in the SAMP8 mouse. Neurosci Biobehav Rev 1998;22:1ŌĆō20.


89. OŌĆÖNeal-Moffitt G, Pilli J, Kumar SS, Olcese J. Genetic deletion of MT1/MT2 melatonin receptors enhances murine cognitive and motor performance. Neuroscience 2014;277:506ŌĆō521.


90. Liu Y, Ni C, Li Z, Yang N, Zhou Y, Rong X, et al. Prophylactic melatonin attenuates isoflurane-induced cognitive impairment in aged rats through hippocampal melatonin receptor 2 - cAMP response element binding signalling. Basic Clin Pharmacol Toxicol 2017;120:219ŌĆō226.


92. Mazzucchelli C, Pannacci M, Nonno R, Lucini V, Fraschini F, Stankov BM. The melatonin receptor in the human brain: cloning experiments and distribution studies. Brain Res Mol Brain Res 1996;39:117ŌĆō126.


93. Wan Q, Man HY, Liu F, Braunton J, Niznik HB, Pang SF, et al. Differential modulation of GABAA receptor function by Mel1a and Mel1b receptors. Nat Neurosci 1999;2:401ŌĆō403.


94. Srinivasan V, Pandi-Perumal SR, Maestroni GJ, Esquifino AI, Hardeland R, Cardinali DP. Role of melatonin in neurodegenerative diseases. Neurotox Res 2005;7:293ŌĆō318.


95. Liu J, Clough SJ, Hutchinson AJ, Adamah-Biassi EB, Popovska-Gorevski M, Dubocovich ML. MT1 and MT2 melatonin receptors: a therapeutic perspective. Annu Rev Pharmacol Toxicol 2016;56:361ŌĆō383.


96. Iwashita H, Matsumoto Y, Maruyama Y, Watanabe K, Chiba A, Hattori A. The melatonin metabolite N1-acetyl-5-methoxykynuramine facilitates long-term object memory in young and aging mice. J Pineal Res 2021;70:e12703.


99. Spinedi E, Cardinali DP. Neuroendocrine-metabolic dysfunction and sleep disturbances in neurodegenerative disorders: focus on AlzheimerŌĆÖs disease and melatonin. Neuroendocrinology 2019;108:354ŌĆō364.


100. Pagano ES, Spinedi E, Gagliardino JJ. White adipose tissue and circadian rhythm dysfunctions in obesity: pathogenesis and available therapies. Neuroendocrinology 2017;104:347ŌĆō363.


102. Zlokovic BV. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron 2008;57:178ŌĆō201.


104. Arbon EL, Knurowska M, Dijk DJ. Randomised clinical trial of the effects of prolonged-release melatonin, temazepam and zolpidem on slow-wave activity during sleep in healthy people. J Psychopharmacol 2015;29:764ŌĆō776.


105. Buckner RL, Snyder AZ, Shannon BJ, LaRossa G, Sachs R, Fotenos AF, et al. Molecular, structural, and functional characterization of AlzheimerŌĆÖs disease: evidence for a relationship between default activity, amyloid, and memory. J Neurosci 2005;25:7709ŌĆō7717.



106. Gorfine T, Assaf Y, Goshen-Gottstein Y, Yeshurun Y, Zisapel N. Sleep-anticipating effects of melatonin in the human brain. Neuroimage 2006;31:410ŌĆō418.


108. Hita-Ya├▒ez E, Atienza M, Gil-Neciga E, Cantero JL. Disturbed sleep patterns in elders with mild cognitive impairment: the role of memory decline and ApoE ╬Ą4 genotype. Curr Alzheimer Res 2012;9:290ŌĆō297.

110. Lemoine P, Zisapel N. Prolonged-release formulation of melatonin (Circadin) for the treatment of insomnia. Expert Opin Pharmacother 2012;13:895ŌĆō905.


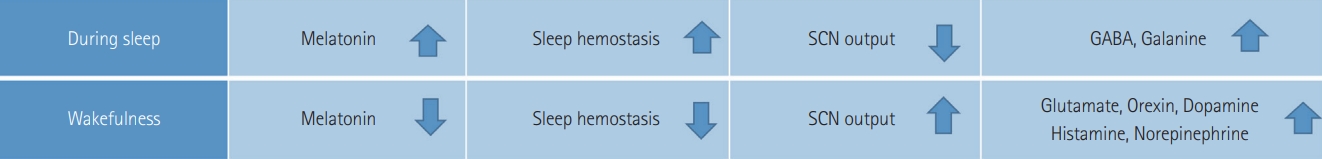
111. Saper CB, Scammell TE, Lu J. Hypothalamic regulation of sleep and circadian rhythms. Nature 2005;437:1257ŌĆō1263.


112. Al-Aama T, Brymer C, Gutmanis I, Woolmore-Goodwin SM, Esbaugh J, Dasgupta M. Melatonin decreases delirium in elderly patients: a randomized, placebo-controlled trial. Int J Geriatr Psychiatry 2011;26:687ŌĆō694.


113. Hatta K, Kishi Y, Wada K, Takeuchi T, Odawara T, Usui C, et al. Preventive effects of ramelteon on delirium: a randomized placebo-controlled trial. JAMA Psychiatry 2014;71:397ŌĆō403.


115. Poeggeler B, Miravalle L, Zagorski MG, Wisniewski T, Chyan YJ, Zhang Y, et al. Melatonin reverses the profibrillogenic activity of apolipoprotein E4 on the Alzheimer amyloid Abeta peptide. Biochemistry 2001;40:14995ŌĆō15001.


116. Trotti LM, Karroum EG. Melatonin for sleep disorders in patients with neurodegenerative diseases. Curr Neurol Neurosci Rep 2016;16:63.


117. McCleery J, Cohen DA, Sharpley AL. Pharmacotherapies for sleep disturbances in AlzheimerŌĆÖs disease. Cochrane Database Syst Rev 2014;(3): CD009178.


118. Lucey BP, Bateman RJ. Amyloid-╬▓ diurnal pattern: possible role of sleep in AlzheimerŌĆÖs disease pathogenesis. Neurobiol Aging 2014;35 Suppl 2:S29ŌĆōS34.


120. Ray CA. Melatonin attenuates the sympathetic nerve responses to orthostatic stress in humans. J Physiol 2003;551(Pt 3):1043ŌĆō1048.

121. Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, Van Someren EJ. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 2008;299:2642ŌĆō2655.


122. Tan DX, Hardeland R, Manchester LC, Poeggeler B, Lopez-Burillo S, Mayo JC, et al. Mechanistic and comparative studies of melatonin and classic antioxidants in terms of their interactions with the ABTS cation radical. J Pineal Res 2003;34:249ŌĆō259.


123. Purves D, Augustine GJ, Fitzpatrick D, Katz LC, McNamara JO, et al. Neuroscience (2nd ed). Sunderland, MA: Sinauer Associates, 2001.
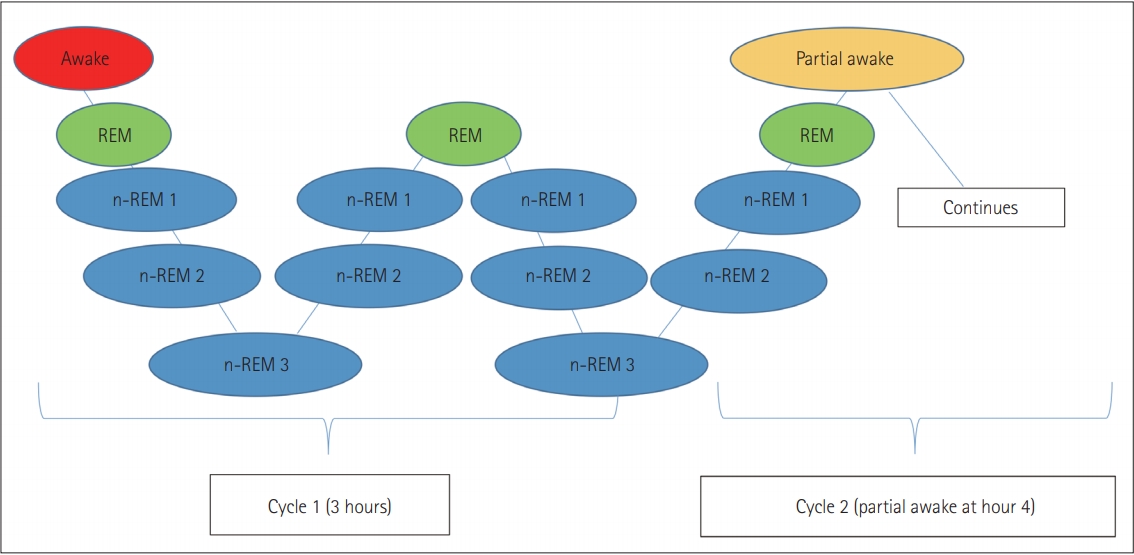
124. Chokroverty S. Overview of sleep & sleep disorders. Indian J Med Res 2010;131:126ŌĆō140.

125. Espa├▒a RA, Scammell TE. Sleep neurobiology for the clinician. Sleep 2004;27:811ŌĆō820.

126. Yang JH, Choi SH, Lee MH, Oh SM, Choi JW, Park JE, et al. Automated assessment of quantitative REM sleep without atonia for diagnosis of REM sleep behavior disorder. Chronobiol Med 2020;2:123ŌĆō128.

127. Richter CP. Biological clocks in medicine and psychiatry: shock-phase hypothsis. Proc Natl Acad Sci U S A 1960;46:1506ŌĆō1530.


128. Hendrickson AE, Wagoner N, Cowan WM. An autoradiographic and electron microscopic study of retino-hypothalamic connections. Z Zellforsch Mikrosk Anat 1972;135:1ŌĆō26.


129. Moore RY, Lenn NJ. A retinohypothalamic projection in the rat. J Comp Neurol 1972;146:1ŌĆō14.


130. Moore RY. Retinohypothalamic projection in mammals: a comparative study. Brain Res 1973;49:403ŌĆō409.


131. Avidan A, Barkoukis T. Review of sleep medicine. Philadelphia: Butterworth-Heinemann, 2007.
132. Kryger M, Roth T, Dement T. Principles and practice of sleep medicine (4th ed). Philadelphia: Saunders, 2005.
133. Koukkou M. Functional states of the brain: their determinants. Amsterdam: Elsevier Science, 1980.
134. Achermann P, Borb├®ly AA. Mathematical models of sleep regulation. Front Biosci 2003;8:s683ŌĆōs693.


139. Xie X, Crowder TL, Yamanaka A, Morairty SR, Lewinter RD, Sakurai T, et al. GABA(B) receptor-mediated modulation of hypocretin/orexin neurones in mouse hypothalamus. J Physiol 2006;574(Pt 2):399ŌĆō414.

140. Li Y, Gao XB, Sakurai T, van den Pol AN. Hypocretin/orexin excites hypocretin neurons via a local glutamate neuronŌĆöa potential mechanism for orchestrating the hypothalamic arousal system. Neuron 2002;36:1169ŌĆō1181.


141. Yamanaka A, Muraki Y, Tsujino N, Goto K, Sakurai T. Regulation of orexin neurons by the monoaminergic and cholinergic systems. Biochem Biophys Res Commun 2003;303:120ŌĆō129.


142. Yamanaka A, Muraki Y, Ichiki K, Tsujino N, Kilduff TS, Goto K, et al. Orexin neurons are directly and indirectly regulated by catecholamines in a complex manner. J Neurophysiol 2006;96:284ŌĆō298.


143. Kumar S, Szymusiak R, Bashir T, Rai S, McGinty D, Alam MN. Effects of serotonin on perifornical-lateral hypothalamic area neurons in rat. Eur J Neurosci 2007;25:201ŌĆō212.


145. Elbaz I, Levitas-Djerbi T, Appelbaum L. The hypocretin/orexin neuronal networks in zebrafish. Curr Top Behav Neurosci 2017;33:75ŌĆō92.


146. Wilson MA, McNaughton BL. Reactivation of hippocampal ensemble memories during sleep. Science 1994;265:676ŌĆō679.


147. Lee AK, Wilson MA. Memory of sequential experience in the hippocampus during slow wave sleep. Neuron 2002;36:1183ŌĆō1194.


148. Peigneux P, Laureys S, Fuchs S, Collette F, Perrin F, Reggers J, et al. Are spatial memories strengthened in the human hippocampus during slow wave sleep? Neuron 2004;44:535ŌĆō545.


149. Maquet P, Laureys S, Peigneux P, Fuchs S, Petiau C, Phillips C, et al. Experience-dependent changes in cerebral activation during human REM sleep. Nat Neurosci 2000;3:831ŌĆō836.


150. Tononi G, Cirelli C. Sleep function and synaptic homeostasis. Sleep Med Rev 2006;10:49ŌĆō62.


151. Kong N, Choi J, Seo WS. Evaluation of sleep problems or disorders using sleep questionnaires. Chronobiol Med 2019;1:144ŌĆō148.

157. Palchykova S, Winsky-Sommerer R, Meerlo P, D├╝rr R, Tobler I. Sleep deprivation impairs object recognition in mice. Neurobiol Learn Mem 2006;85:263ŌĆō271.


158. Prince TM, Wimmer M, Choi J, Havekes R, Aton S, Abel T. Sleep deprivation during a specific 3-hour time window post-training impairs hippocampal synaptic plasticity and memory. Neurobiol Learn Mem 2014;109:122ŌĆō130.


160. Stepanski EJ. The effect of sleep fragmentation on daytime function. Sleep 2002;25:268ŌĆō276.


161. Gupta CC, Centofanti S, Dorrian J, Coates A, Stepien JM, Kennaway D, et al. Altering meal timing to improve cognitive performance during simulated nightshifts. Chronobiol Int 2019;36:1691ŌĆō1713.


162. Mitler MM, Lund R, Sokolove PG, Pittendrigh CS, Dement WC. Sleep and activity rhythms in mice: a description of circadian patterns and unexpected disruptions in sleep. Brain Res 1977;131:129ŌĆō145.


167. Vyazovskiy VV, Walton ME, Peirson SN, Bannerman DM. Sleep homeostasis, habits and habituation. Curr Opin Neurobiol 2017;44:202ŌĆō211.


168. Gupta CC, Dorrian J, Grant CL, Pajcin M, Coates AM, Kennaway DJ, et al. ItŌĆÖs not just what you eat but when: the impact of eating a meal during simulated shift work on driving performance. Chronobiol Int 2017;34:66ŌĆō77.


169. Foster RG, Wulff K. The rhythm of rest and excess. Nat Rev Neurosci 2005;6:407ŌĆō414.


171. Wulff K, Gatti S, Wettstein JG, Foster RG. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci 2010;11:589ŌĆō599.


172. Cho CH, Lee Y. The chronobiologic-based practical approach to shift work. Chronobiol Med 2019;1:103ŌĆō106.

173. Straif K, Baan R, Grosse Y, Secretan B, El Ghissassi F, Bouvard V, et al. Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol 2007;8:1065ŌĆō1066.


174. Park TJ, Paek DM, Joh KO, Park JS, Cho SI. The relationship between shift work and work-related injuries among Korean workers. Korean J Occup Environ Med 2012;24:52ŌĆō60.

175. Hunter CM, Figueiro MG. Measuring light at night and melatonin levels in shift workers: a review of the literature. Biol Res Nurs 2017;19:365ŌĆō374.


177. Grundy A, Sanchez M, Richardson H, Tranmer J, Borugian M, Graham CH, et al. Light intensity exposure, sleep duration, physical activity, and biomarkers of melatonin among rotating shift nurses. Chronobiol Int 2009;26:1443ŌĆō1461.


178. Choukroun J, Geoffroy PA. Light therapy in mood disorders: a brief history with physiological insights. Chronobiol Med 2019;1:3ŌĆō8.

179. Grundy A, Tranmer J, Richardson H, Graham CH, Aronson KJ. The influence of light at night exposure on melatonin levels among Canadian rotating shift nurses. Cancer Epidemiol Biomarkers Prev 2011;20:2404ŌĆō2412.


180. Papantoniou K, Pozo OJ, Espinosa A, Marcos J, Casta├▒o-Vinyals G, Basaga├▒a X, et al. Circadian variation of melatonin, light exposure, and diurnal preference in day and night shift workers of both sexes. Cancer Epidemiol Biomarkers Prev 2014;23:1176ŌĆō1186.