Factor Associated With Sleep Disturbance and Its Consequence in Jet-Lagged Employee
Article information
Abstract
Objective
The current study aims to explore the determinants of sleep disturbance (insomnia and daytime sleepiness) and its potential consequence (depression, somatization, fatigue, and cognitive failure) on jet-lagged employee.
Methods
One-hundred twenty JLEs (49 males and 71 females) completed an online survey. The survey asked for information regarding jet lag and administered eight self-report questionnaires: Ford Insomnia Response to Stress Test for sleep reactivity, Glasgow Sleep Effort Scale for dysfunctional sleep efforts, Insomnia Severity Index for insomnia, Epworth Sleepiness Scale for daytime sleepiness, Center for Epidemiologic Studies-Depression scale for depression, Somatization Subscale of the Symptom Checklist 90-item for somatic symptoms, Fatigue Severity Scale for fatigue, and Cognitive Failure Questionnaire for cognitive impairments.
Results
Higher sleep reactivity (β=0.45, p<0.001) and sleep effort (β=0.40, p<0.001) significantly predicted insomnia. Higher sleep reactivity (β=0.40, p<0.01) significantly predicted sleepiness. Higher insomnia and sleepiness significantly predicted depression (β=0.50, p<0.001, β=0.22, p<0.01, respectively) and somatic symptoms (β=0.46, p<0.001, β=0.22, p<0.01, respectively). Flight time per flight (β=0.22, p<0.01), higher sleep reactivity (β=0.20, p<0.05), and higher insomnia severity (β=0.43, p<0.001) significantly predicted fatigue. Higher sleep reactivity significantly predicted cognitive failure (β=0.35, p<0.001).
Conclusion
This current study reports that sleep reactivity and sleep efforts of JLEs are associated with their sleep disturbances more than other flight-related factors. Sleep disturbances of JLEs are associated with increase depression, somatization, and fatigue. Sleep reactivity caused by stressful situation are associated with fatigue and cognitive impairments of JLE. The current study suggests that management of sleep and stress may be helpful for the mental and physical well-being of JLE.
INTRODUCTION
Jet lag is considered to be a range of symptoms such as daytime sleepiness or difficulty in starting or maintaining sleep [1,2]. Jet lag results from a mismatch between internal biological time and environmental time caused by rapid eastward or westward travel across multiple time zones [3]. In particular, frequent night flights and mismatch with one’s normal body rhythm may cause sleep disturbance including insomnia and daytime sleepiness, and lead to fatigue, drowsiness, sensitivity, and decreased work ability [1,4]. Unfamiliar sleep environments and small circadian shifts which jet lag employees can experience under their working environment can produce transient sleep difficulties [5]. In this study, the term jet-lagged employees (JLEs) is used to describe employees working in job conditions that make them more susceptible to jet lag.
Sleep reactivity is one of the factors contributing to the onset and the maintenance of insomnia [6]. Sleep reactivity is the degree to which individuals exhibit acute sleep-disruptive responses to stress [7]. Until now, studies on the sleep reactivity of employees who experience jet lag on a regular basis due to their work has not been done. Shift workers, including employees who experience jet lag, have higher job-related stress than compared with day workers [8].
Behaviors and cognitions of people with insomnia often involve high sleep effort, which may be manifested as performance anxiety about sleep, a need for sleep control, and/or trying to sleep too hard. Workers who need to change sleep pattern frequently due to their work, tend to worry about sleep and may want to control sleep more than regular day time workers [9]. Sleep effort is also one factor involved in maintaining insomnia by interfering with the natural process that regulates sleep by increasing arousal before sleep [10].
Disruption of circadian rhythm impairs physical and mental health [11], and JLEs such as cabin crew members, who have chronically and frequently experienced circadian rhythm disturbance, may also experience cognitive impairments like working memory deficits [12]. This current study aims to explore the determinants of sleep disturbance (insomnia and daytime sleepiness) and its potential consequence (depression, somatization, fatigue and cognitive impairment) in JLEs.
METHODS
Participants
One-hundred twenty JLEs (36.32±8.63 years, 49 males and 71 females) were recruited through online advertisement and online survey company. Ninety-seven participants (80.8%) were flights attendants, while twenty-three (19.2%) had other jobs needing frequent jet-lag as mate, travel guide, international buyer, or foreign language interpreter.
The inclusion criteria were age at least 18 years old and having a full-time job requiring repetitive travel across multiple time zones which makes them more susceptible to jet lag. Participants whose number of cross time zone flight was less than 1 per month were excluded.
All participants gave written informed consent. All procedures were conducted in accordance with the ethical standards of our national and institutional committees on human experimentation and the Helsinki Declaration of 1964 (as revised in 2013). The study protocol was approved by the Institutional Review Board of Samsung Medical Center (approval no. 2019-04-095).
Questionnaires
All questionnaire were provided online. Information regarding the flight and the jet lag were self-reported. Cross time zone flight per month, average flight time per flight, and average sleep time during flights were asked. Four sleep-related questionnaires were used in the current study. The Ford Insomnia Response to Stress Test (FIRST) was used for assessing sleep reactivity [13]. FIRST is a self-report questionnaire consists of items examining the likelihood that a person would experience sleep disturbance in response to 9 hypothetical stressful situations. The Glasgow Sleep Effort Scale (GSES) measures the core components of an overall model on persistent preoccupation with sleep [14]. GSES consists of 7 items manifesting the individual’s effort to sleep. The Epworth Sleepiness Scale (ESS) is a well-validated self-administered questionnaire assessing the subjective level of daytime sleepiness in 8 common situations [15]. The Insomnia Severity Index (ISI) is a commonly used 7-item self-report questionnaire measuring the severity of both daytime and nighttime symptoms of insomnia [16].
For assessing mood, somatization, fatigue, and cognition, four self-report questionnaires were also used. The Korean version of short form of Center for Epidemiologic Studies-Depression scale (CES-D) was used in the current study to evaluate depressive symptoms [17]. The short-form of CES-D is composed of 11 items, which have the same constructs with the original. The Korean version of the short-form of CES-D has acceptable internal consistency and validity, comparable to the original. To evaluate the impact of fatigue on study participants, the Korean version of Fatigue Severity Scale (FSS) was used [18]. FSS includes 9 items, which explore motor aspects of fatigue, daytime impairment by fatigue, and vulnerability to fatigue. Korean version of FSS has decent reliability and test-retest variability. To evaluate somatization symptoms of participants, the Korean version of the somatization subscale of the Symptom Checklist 90-item version (SCL-SOM) was used [19]. SCL-90-R is composed of 12 questions, which are designed to assess subjective distress of bodily dysfunction [20]. The Korean version of SCL has good reliability and validity [21]. Cognitive efficiency was assessed using the Korean version of the Cognitive Failure Questionnaire (CFQ) [22]. The CFQ is a self-reported questionnaire that assesses failures of memory, action, and perception in everyday life. It consists of 25 self-rated items; scores range between 0 and 100.
Statistics
Among-group differences in continuous variables were compared using the independent t-test. Correlation analysis were also conducted to examine the relationships between dimensional variables. Two stepwise regressions were used in the current study. The first regression models were for exploring the determinants of sleep disturbances of participants (dependent variable; ISI or ESS, independent variables: age, sex, flight time per flight, sleep time during flights, FIRST, and GSES). Variables which were associated with jet-lag flight or vulnerability to sleep disturbances were set as independent variables, while variables representing sleep disturbance itself were set as dependent variables. The second regression models were for exploring the determinants of consequence of sleep disturbances and jet-lag flights (dependent variable: CES-D, SCL-SOM, FSS, or CFQ; independent variables: age, sex, time zone flight per month, flight time per flight, sleep time during flights, FIRST, GSES, ISI, and ESS). Variables which were associated with jet-lag flight, or sleep disturbances were set as independent variables, while variables representing potential effects of jet lag sleep disturbances were set as dependent variables. All statistical analysis were done using SPSS, version 27 (IBM Corp., Armonk, NY, USA).
RESULTS
Demographic and flight-related variables were represented in Table 1. The mean age of participants was 36.32±8.63 years. There were 49 males (40.8%) and 71 females (59.2%). Females (33.58±7.56 years) were younger than males (40.29±8.62 years) (t=4.51, p<0.01). Ninety-three participants (77.5%) had more than 3 flights across the time zone per month. The average flight time per flight of 102 participants (85.0%) were more than 4 hours per flight. The average sleep time during flight of 108 participants (90.0%) were less than 5 hours per flight. Females had more flights per month (t=2.56, p=0.12) and less sleep time during flight (t=2.03, p=0.05) than males. Younger age was correlated with more flights per month (r=0.27, p<0.01).
Sleep, mood, somatization, fatigue, and cognition of participants were represented in Table 2. Females also showed higher FIRST (t=2.51, p=0.01) and GSES (t=2.49, p=0.01) scores compared to males. Males showed higher ESS (t=2.01, p=0.05) compared to females. Younger age was correlated with higher FIRST (r=0.19, p=0.04) and higher GSES (r=0.30, p<0.01). The number of flights per month was correlated with higher ESS (r=0.20, p=0.03). The average flight time per flight was correlated with higher FSS (r=0.20, p=0.02). All variables regarding sleep and mood (i.e., FIRST, GSES, ESS, ISI, CES-D, SCL-SOM, FSS, and CFQ) showed positive correlation with each other, except that ESS had no significant correlation with GSES and FSS.
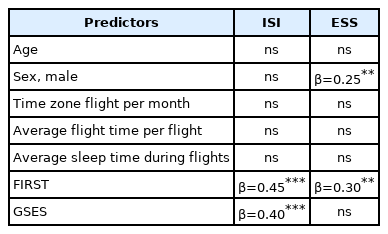
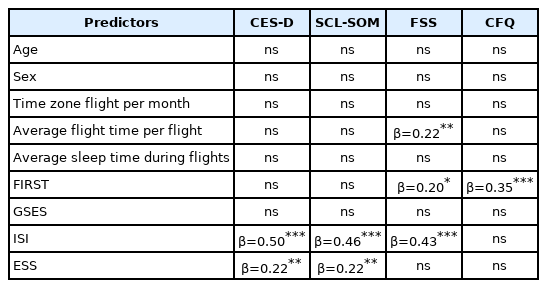
Predictors of insomnia and sleepiness were presented in Table 3. In the stepwise regression model for predicting insomnia, higher sleep reactivity (β=0.45, p<0.001) and sleep effort (β=0.40, p<0.001) significantly predicted insomnia. Male sex (β=0.25, p<0.01) and higher sleep reactivity (β=0.30, p<0.01) significantly predicted sleepiness. Predictor of mood, somatic symptoms, fatigue, and cognition failure were presented in Table 4. In the stepwise regression model for predicting depression, higher insomnia severity (β=0.50, p<0.001) and sleepiness (β=0.22, p<0.01) significantly predicted depression. Higher insomnia severity (β=0.46, p<0.001) and sleepiness (β=0.22, p<0.01) significantly predicted somatic symptoms. Flight time per flight (β=0.22, p<0.01), higher sleep reactivity (β=0.20, p<0.05) and higher insomnia severity (β=0.43, p<0.001) significantly predicted fatigue. Higher sleep reactivity significantly predicted cognitive failure (β=0.35, p<0.001).
DISCUSSION
The current study explored the determinants of sleep disturbance (insomnia and daytime sleepiness) and its potential consequence (depression, somatization, fatigue, and cognitive failure) in jet-lag employees. Higher sleep reactivity and sleep effort significantly predicted severity of insomnia in jet-lag employees. Higher sleep reactivity significantly predicted sleepiness in jet-lag employees. Related to its potential consequence, high insomnia severity and sleepiness significantly predicted depression and somatic symptoms. Furthermore, higher sleep reactivity was significantly predictive of cognitive failure. Flight time per flight, higher sleep reactivity, and higher insomnia severity significantly predicted fatigue severity.
Higher sleep reactivity and sleep effort significantly predicted severity of insomnia in jet-lag employees. The current study is the first to report the sleep reactivity and sleep effort on particularly jet-lag employees. This result is consistent with previous studies which reported that the higher sleep reactivity and sleep effort may contribute to the of insomnia exist development onset and maintenance [6]. High sleep reactivity (i.e., sleep systems easily disrupted by stress) have been shown to be at high risk for developing insomnia as compared to those with low sleep reactivity (i.e., more robust sleep systems). Especially, for jet-lag employees have more occupational stress [23] and previous studies have shown that stress system interacted with or even impinged on circadian regulation [24,25]. It suggests that in jet-lag employees, coping skill for stress may be difficult to function properly due to circadian misalignment [26]. Additionally, it is likely that increased sleep reactivity and sleep effort can produce arousal and sleep delay, which can accelerate the onset of sleep disturbances [27].
Previous studies have been reported that excessive sleepiness and insomnia is the one of the most common consequences in shift workers [28,29]. Ohayon et al. [30] reported that sleepiness was more related to short sleep duration rather than to work schedule, but it was not clear whether it is related to sleep reactivity. The current study showed that sleep reactivity predicted sleepiness in jet-lag employees, and it suggests the addressing sleep reactivity can decrease sleepiness at least in this population. The current study also showed insomnia and sleepiness predicted depression and somatic symptoms in jet-lag employees. From a mental health perspective, generally rotating shift workers which can be classified as rapid shifting or slow shifting are more experience psychiatric disease and greater psychosocial distress, such as depression and anxiety [13,31]. Our results consistent with previous studies and contributes to clarifying the possible psychological consequences of depression and somatic symptoms in a group of jet lag-fatigue employees.
Our findings provide new evidence about relationship of the sleep reactivity and cognitive failure. In the current study, higher sleep reactivity predicted cognitive failure in jet-lag employees. Although controversial, recent works have suggested the circadian activity rhythms may affect to cognitive vulnerabilities and even impairment in memory, attention, information processing ability due to circadian misalignment [32,33]. Additionally, some studies suggested the jet lag and rotational shift tasks can result in a temporary loss of phase coherence between individual brain clocks and impaired circadian coordination, leading to decreased optimal cognitive performance [34,35]. In this regard, our findings are not only consistent with earlier works but also indicating that individuals who have a chronic irregular circadian system with sleep reactivity may lead cognitive failure.
Unlike sleepiness which means increased sleep propensity, fatigue is a subjective feeling of physical and/or mental tiredness [36]. Fatigue in flight attendant has been reported to be associated with insomnia and external work-related factors such as flight hours and debriefing hours [37-39]. However, to the best of our knowledge, this is the first study to explore the relationship of not only just the flight time and insomnia severity but also sleep reactivity and fatigue in participants who experience jet lag. This study indicate that particular psychological factors may well be relevant in the jet-lag employee’s fatigue severity.
Despite the implications of our study, several limitations should be noted. Although our study suggested the influence of psychological factors on insomnia and daytime sleepiness, the design in this study could not fully delineate the complex interactive relationship among sleep reactivity and sleep effort. Also, as this study was cross-sectional in nature, we cannot explore temporal or causal associations between jet lag exposure, on the one hand, and sleep reactivity, sleep effort and also the potential consequences, on the other. We also relied on self-reported answers to online questionnaires. A future study should investigate whether the results are replicated when objective tools such as actigraphy and polysomnography are employed.
In conclusion, this current study reported that higher sleep reactivity and sleep effort predicted the insomnia severity in employees who experience jet lag. In addition, higher sleep reactivity predicted sleepiness. Insomnia severity and sleepiness predicted depression and somatic symptoms. Higher sleep reactivity also predicted cognitive failure. Flight time per flight, higher sleep reactivity and insomnia predicted fatigue severity. This current study suggests that management of sleep and stress may be helpful for the mental and physical well-being of JLEs.
Notes
Funding Statement
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2022R1A2C2008417), the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2020M3E5D9080561), and a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (No. HR21C0885).
The authors have no potential conflicts of interest to disclose.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Seog Ju Kim. Data curation: Hyeyeon Jang, Seog Ju Kim. Formal analysis: Hyeyeon Jang, Seog Ju Kim. Investigation: Hyeyeon Jang, Seog Ju Kim. Methodology: Hyeyeon Jang, Seog Ju Kim. Project administration: Seog Ju Kim. Resources: Seog Ju Kim. Software: Hyeyeon Jang, Seog Ju Kim. Supervision: Seog Ju Kim. Validation: Seog Ju Kim. Visualization: Hyeyeon Jang. Writing—original draft: Hyeyeon Jang. Writing—review & editing: Seog Ju Kim.