Poor Sleep Quality, Eveningness, and Anxiety Are Associated With Internet/Smartphone Addiction in Korean Adolescents
Article information
Abstract
Objective
Internet addiction and smartphone addiction are emerging mental health concerns in adolescents. To determine the factors related to these conditions, we investigated their associations with sleep quality, chronotype, sleep patterns, daylight exposure, depression, and anxiety.
Methods
Self-rated questionnaires, including the Internet Addiction Proneness Scale-Short Form, Smartphone Addiction Scale–short version, Insomnia Severity Index, Morningness–Eveningness Questionnaire, Epworth Sleepiness Scale, sleep-related questionnaires, and Hospital Anxiety and Depression Scale, were administered in a study population of 1,610 Korean high school students. Multiple linear regression analyses were performed to evaluate the associations with internet addiction and smartphone addiction.
Results
Multiple linear regression showed significant associations of internet addiction with poor sleep quality (β=0.094, p<0.001), eveningness (β=-0.071, p=0.006), less daylight exposure (β=-0.066, p=0.005), anxiety (β=0.252, p<0.001), and older age (β=0.295, p<0.001). Smartphone addiction was significantly associated with poor sleep quality (β=0.076, p=0.005), eveningness (β=-0.164, p<0.001), excessive daytime sleepiness (β=0.109, p<0.001), longer time in bed on weekdays (β=0.057, p=0.024), shorter weekend oversleep (β=-0.081, p=0.005), anxiety (β=0.192, p<0.001), and younger age (β=-0.145, p<0.001).
Conclusion
Our findings suggest that poor sleep quality, eveningness, and anxiety can serve as predictors of both internet addiction and smartphone addiction in adolescents. Internet addiction seems to be negatively associated with daylight exposure, whereas smartphone addiction showed significant associations with sleep patterns. Additional studies regarding the causal relations between these factors are needed.
INTRODUCTION
Internet addiction has been shown to disrupt the daily life of adolescents. Excessive and uncontrollable internet use may lead to serious mental health problems, including sleep problems and emotional dysregulation, and may also have negative effects on academic function and social relationships [1,2]. Specifically, internet addiction may act as a potential risk factor for developing internet game addiction, and there is concern regarding cyber bullying and various crimes associated with the dependence of adolescents on social networking services. Internet addiction is characterized by excessive or uncontrollable desires and behaviors for internet use and has a disruptive influence on various aspects of daily life. Recent studies demonstrated that internet addiction is associated with sleep problems, a disturbed circadian rhythm, depression, and anxiety in adolescents [2-4]. Moreover, sleep disturbances and internet addiction may affect suicidal ideation among depressive adolescents [5].
Internet use has increasingly been taking the form of smartphone use, and the number of smartphone devices per person in South Korea reached 0.94 in 2021 [6]. Among junior high school students in Japan, smartphone use was reported to be one of the most important factors contributing to internet addiction [7]. Therefore, it is necessary to identify factors that can predict not only internet addiction but also smartphone addiction. Smartphone addiction can be defined as cravings for smartphones, withdrawal, and tolerance, which can significantly disrupt daily life. Smartphone addiction is also related to sleep problems, a disturbed circadian rhythm, depression, and anxiety, but most evidence reported to date has been based on adults [8-10].
Internet addiction is dangerous in itself in that individuals may be exposed to excessively provocative content over a long time, but smartphone addiction may have discriminating psychopathology in that smartphones enable easier access to media and allow the user to receive an instant response from others. Therefore, it is necessary to identify the disease-modifying factors associated not only with internet addiction, but also with smartphone addiction. To our knowledge, however, there have been no studies regarding the factors associated with both internet and smartphone addiction in adolescents.
This study was performed to evaluate the associations between sleep quality and internet/smartphone addiction independently in a population of adolescent Korean high school students. In addition, this study also investigated whether morningness-eveningness could predict internet/smartphone addiction, and assessed the associations of daytime sleepiness, daylight exposure, depression, and anxiety with internet/smartphone addiction.
METHODS
Participants
This study was performed as part of a local child/adolescent sleep health survey conducted by Haman-gun Community Mental Health Center, Gyeongsang Province, South Korea. A total of 1,610 students ranging in age from 15 to 19 years were recruited from five high schools in Haman-gun. The participants were asked to complete questionnaires about problematic internet and smartphone use, emotional problems, and sleep patterns. Written informed consent was obtained from all students, parents, and teachers participating in the study. All study protocols were approved by the Institutional Review Board of Gyeongsang National University Hospital (IRB file number: 2015-06-004-004).
Assessments
Internet Addiction Proneness Scale–short form
The Internet Addiction Proneness Scale–short form (IAPS-SF) is the short version of the Internet Addiction Proneness Scale, developed by the Korean Ministry of Science and ICT to improve its clinical applicability. The IAPS-SF consists of 20 items on seven subfactors: distance of adaptive functions, distance of reality testing, additive automatic thought, withdrawal, virtual interpersonal relationships, deviant behavior, and tolerance. Subjects can be classified according to the standardized total score into high-risk users (score: ≥70), potential-risk users (score: 63–69), or general users (score: <63). In the case of Korean high school students, a total score ≥52 points is classified as indicating high risk and a score ≥47 points is classified as indicating potential risk. The IAPS-SF has been standardized and verified for its validity and reliability in Korea [11].
Smartphone Addiction Scale–short version
The Smartphone Addiction Scale–short version (SAS-SV) is the short version of the original Smartphone Addiction Scale (SAS), which consists of 33 items that evaluate six characteristics of problematic smartphone use: disturbance of adaptive functions, addictive automatic thought, withdrawal, virtual interpersonal relationships, overuse, and tolerance. The SAS-SV has been standardized and verified for its validity and reliability in Korea [12]. This self-reported scale includes 10 items, each scored on a 6-point Likert scale with higher scores indicating a higher level of smartphone addiction. Male subjects with a total score ≥31 points and female subjects with a total score ≥33 points are classified as having smartphone addiction problems.
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS) includes two subscales: Hospital Anxiety and Depression-Anxiety (HAD-A) and Hospital Anxiety and Depression-Depression (HAD-D). A total of 14 items are included with seven items each for depression and anxiety subscales, which allows clinicians to assess the most common emotional symptoms rapidly and simply. Each item is scored from 0 to 3 on a 4-point Likert scale, with higher scores indicating higher levels of anxiety and depression [13]. A total subscale score ≥8 points indicates considerable anxiety or depression symptoms. The Korean version of the HADS has been verified for validity and reliability [14].
Sleep-related questionnaires
All participants completed sleep-related questionnaires assessing information about sleep patterns and sleep problems. The surveys included sleep parameters such as time in bed (TIB) and total sleep time (TST), which were used to evaluate weekend oversleep and social jetlag, calculated by the absolute value of the difference in the midpoint of sleep times between weekdays and weekends. In addition, we collected data on the mean daytime sunlight exposure represented by the duration of any outside activity performed between 10:00 and 15:00 on weekdays and weekends. Such time around midday was considered because early morning and late evening light exposure both lead to circadian phase shifting, and the time interval of 10:00 to 15:00 is generally considered to be the optimal time of sunlight exposure for the effective synthesis of vitamin D [15,16]. Sunlight exposure between 10:00 and 15:00 has been reported to be one of the predictors of morningness in the previous study [17].
Insomnia Severity Index
The Insomnia Severity Index (ISI) assesses the quality of sleep on a seven-item scale. Each item is scored on a 5-point Likert scale (0–4), with a higher total score indicating poorer sleep quality. The ISI has been validated for the clinical measurement of insomnia severity [18]. The Korean version of the ISI has been confirmed as a reliable and valid instrument for use in the Korean population [19].
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS), in which participants rate their chances of dozing off or falling asleep while engaged in eight different situations, is used to measure excessive daytime sleepiness. Each item is scored on a 4-point Likert scale (0–3), with a higher total score indicating more severe daytime sleepiness. An ESS score of 0–10 indicates normal daytime sleepiness and a score of 11–24 indicates a high level of daytime sleepiness for which medical attention is recommended. An ESS score ≥16 suggests sleep disorders, including insomnia, obstructive sleep apnea, and narcolepsy. We used the Korean version of the ESS, which has been validated in the Korean language [20].
Morningness–Eveningness Questionnaire
The Morningness–Eveningness Questionnaire (MEQ) assesses the alertness and preferred time for sleep and waking in terms of circadian rhythm. The scale can be used to determine chronotype through 19 questions, with higher scores indicating a tendency for higher morningness and lower eveningness [21]. The MEQ has been verified for validity and reliability, and the Korean version has also been verified for its reliability and validity [21,22].
Statistical analysis
Correlations between continuous variables were analyzed according to the Pearson’s correlation coefficients. Differences between groups were evaluated by the independent t-test. Multiple linear regression analyses were performed to predict proneness for internet addiction controlling for age, sex, sleep parameters, sleep-related questionnaire scores, and depression/anxiety symptoms. Additional multiple linear regression analyses were performed to predict smartphone addiction. All of the analyses were performed using SPSS Windows Ver. 25 (IBM Corp., Armonk, NY, USA). In all analyses, p<0.05 was taken to indicate statistical significance.
RESULTS
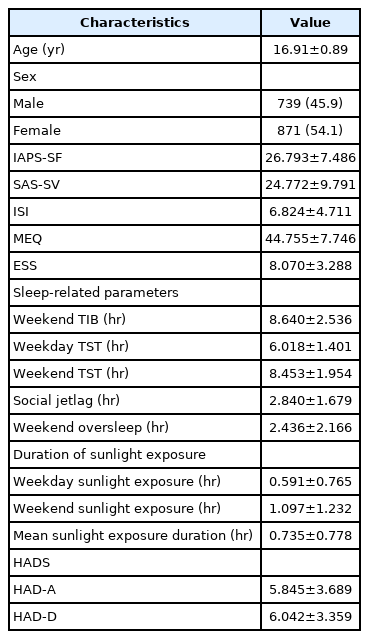
The study population consisted of 1,610 students from five high schools in Haman-gun. The demographic characteristics, sleep parameters, and other clinical information are presented in Table 1. The mean total IAPS-SF and SAS-SV scores were 26.793±7.486 and 24.772±9.791, respectively. Male students showed greater proneness to internet addiction (t=-10.34, DF=1,410.61, p<0.001), while female students showed greater proneness to smartphone addiction (t=7.327, DF=1,608, p<0.001).
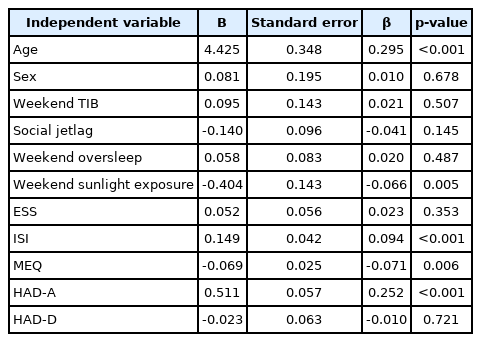
To identify predictive factors of internet addiction, a multiple linear regression analysis was conducted with age, sex, sleep parameters, and questionnaire scores as independent variables (Table 2). Older age (β=0.295, t=12.698, p<0.001) and less weekend sunlight exposure (β=-0.066, t=-2.823, p=0.005) were significantly associated with higher risk of internet addiction, whereas sex (β=0.010, t=0.415, p=0.678) and weekend oversleeping (β=0.020, t=0.695, p=0.487) showed no such relations. With regard to sleep- and mood-related questionnaires, higher internet addiction proneness was predicted by poor sleep quality (β=0.094, t=3.548, p<0.001), eveningness (β=-0.071, t=-2.746, p=0.006), and higher anxiety level (β=0.252, t=8.892, p<0.001).
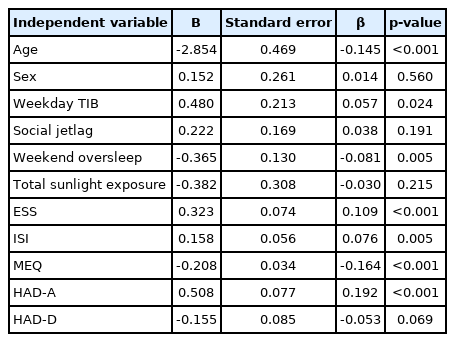
Another multiple linear regression analysis was performed with SAS-SV score as the dependent variable to identify predictive factors of smartphone addiction (Table 3). Younger age (β=-0.145, t=-6.082, p<0.001), longer TIB on weekdays (β=0.057, t=2.254, p=0.024), shorter amount of oversleeping on weekends (β=-0.081, t=-2.803, p=0.005), excessive daytime sleepiness (β=0.109, t=4.348, p<0.001), poor sleep quality (β=0.076, t=2.813, p=0.005), and eveningness in the MEQ (β=-0.164, t=-6.151, p<0.001) were significantly associated with a higher risk of smartphone addiction, as represented by a higher SAS-SV score. Sex did not show significant associations with smartphone addiction (β=0.014, t=0.583, p=0.560). Higher anxiety level was also significantly associated with higher SAS-SV score (β=0.192, t=6.617, p<0.001).
DISCUSSION
This study identified factors associated with internet and smartphone addiction among adolescents in Korea, including sleep quality, chronotype, other sleep-related factors, and anxiety. The findings suggest that poor sleep quality and eveningness are both associated with a higher risk of smartphone addiction and internet addiction. Higher anxiety was also associated with problems of both internet addiction and smartphone addiction. Students with greater smartphone addiction spent longer times in bed on weekdays and reported higher levels of daytime sleepiness. Students with greater internet addiction had less sunlight exposure during the daytime.
Consistent with several previous reports, the present study showed that poor sleep quality was significantly associated with internet addiction in adolescents. Kawabe et al. [7] reported that Japanese high school students with internet addiction showed higher sleep disturbance scores. In a recent cross-sectional school-based study in Nepal, Karki et al. [2] found that internet addiction was significantly associated with poor sleep quality as assessed by the Pittsburgh Sleep Quality Index (PSQI). In another cross-sectional study of 600 university students, significant correlations were found between internet addiction and insomnia [23]. One longitudinal study in a population of 1,253 children and adolescents assessing the relations of a wide arrange of sleep problems, including early/middle insomnia, circadian rhythm, and sleep-related behaviors, with internet addiction showed that early and middle insomnia were predictive factors of internet addiction and that internet addiction was predictive of a disturbed circadian rhythm [3]. Moreover, eveningness was shown to predict internet addiction in the present study, consistent with previous reports. For example, Lin and Gau [24] reported that eveningness was associated with increased compulsive internet use in a population of 2,731 college students in Taiwan. Morningness-eveningness chronotype serves as a significant predictor of various sleep problems and sleep quality, which in turn affect mental health, in adolescents [25,26]. Taken together, these findings indicate that interventions, such as inference-based cognitive-behavioral therapy focusing on improving sleep quality or the normalization of circadian rhythms, may play an important role in improving internet addiction.
The present study also demonstrates that students with higher levels of anxiety are more prone to problematic internet use. Gao et al. [4] suggested that adolescents with depression and anxiety have an increased risk of developing internet addiction. Several other studies showed that anxiety symptoms were significantly associated with compulsive internet use, and anxiety was also shown to be a risk factor for internet addiction [23,24,27]. Depression showed a negative correlation with internet addiction, although this was not statistically significant in the present study. Previous studies have yielded discrepant results regarding the association between depression and internet addiction. One study showed that depression and anxiety are risk factors for internet addiction [4], while another showed that depression was a protective factor against smartphone addiction [27]. The present study suggests that anxiety plays a more important role than depression in the psychopathology underlying the development of internet addiction in adolescents.
Another important finding of our study is the association between sunlight exposure and internet addiction. Our results show that students with less daytime sunlight exposure during the weekends had higher levels of internet addiction. The role of daylight exposure in the circadian rhythm involving intrinsic photosensitive retinal ganglion cells is widely established to be associated with mood, cognition, and sleep [28]. In a study assessing the relationship between circadian typology and resilience, a regression analysis with sunlight exposure included as one of the morningness-related modifiable behavioral features in a Korean college student population showed that the mean amount of sunlight exposure was a positive predictor of morningness and contributed to promoting resilience [17]. However, there has been little research focusing on the relationship between psychopathology and sunlight exposure in adolescents, and to our knowledge, ours is the only study to date to show an association between sunlight exposure and internet addiction. The significant association with daytime sunlight exposure during weekends may be due to the lifestyle of general Korean high school students, who generally remain in school buildings between 10:00 and 15:00, which can make sunlight exposure during weekdays less discriminative.
The present study shows that poor sleep quality is significantly associated with smartphone addiction in adolescents. Two previous studies of medical school students in India showed a positive correlation between sleep quality and smartphone addiction [29,30]. Another study of university students revealed that level of smartphone use was positively correlated with subjective poor sleep quality [8]. All three studies assessed sleep quality using the PSQI, whereas we used the ISI in the present study [8,29,30]. In addition, these previous studies were performed with a population of medical school or university students, who tend to represent a more highly educated population. In one systematic review regarding children and young people, Sohn et al. [10] reported that problematic smartphone use was significantly associated with poorer sleep quality. The results of the present study confirm that poor sleep quality could predict smartphone addiction. Moreover, ISI appears to be a convenient and valid instrument for assessing this association in a general school setting.
In the present study, eveningness was also shown to predict smartphone addiction. One study of the association between chronotype and smartphone addiction proneness in German adolescents reported that eveningness as evaluated by the Composite Scale of Morningness was an important predictor of smartphone addiction, in which the association was even stronger than that of sleep duration [9]. In another study performed in a population of medical university students, Randjelovic et al. [31] reported that students with problematic smartphone use were more frequently classified as having the evening chronotype. As poor sleep quality and eveningness could also predict internet addiction, both internet and smartphone use can be expected to share the same pathophysiology regarding the circadian rhythm.
In addition, the present study shows that excessive daytime sleepiness could also predict smartphone addiction. Although daytime sleepiness is highly associated with students’ academic performance, and more importantly with depression, a limited number of studies have approached the direct association between daytime sleepiness and smartphone addiction [32]. In a previous multivariate analysis involving 1,796 Korean adolescents, students who reported that they “did not feel refreshed in the morning” showed a higher risk of smartphone addiction [33]. In addition, the at-risk smartphone user group was associated with higher daytime sleepiness in students with several factors, such as female sex, alcohol consumption, poor self-perceived health level, initiating sleep after midnight, longer time taken to fall asleep, and duration of night sleep less than 6 h [34]. As excessive daytime sleepiness is considered to be associated with the eveningness chronotype, insomnia, and several emotional and behavioral difficulties in adolescents, further attention should be paid to daytime sleepiness in relation to smartphone addiction [34].
In the present study, students who spent more TIB during weekdays and those with shorter weekend oversleep times were more likely to have a smartphone addiction. Smartphone use in bed may contribute to more TIB, and a previous analysis showed that smartphone use before bedtime had both direct and indirect relations with smartphone addiction [35]. Lemola et al. [36] reported the association between sleep disturbance and use of electronic devices in bed before sleep. To clarify the causal relationship, additional studies including an investigation of adolescents’ bedtime smartphone use and sleep problems in the smartphone addiction group are needed. There have been few other studies regarding the relation of weekend oversleeping with smartphone addiction.
As with the results for internet addiction, higher anxiety was predictive of smartphone addiction in the present study. Whereas depression lacked statistical significance in predicting smartphone addiction in the present study, several previous reports concluded that both depression and anxiety are significantly associated with smartphone addiction. Matar Boumosleh and Jaalouk [37] reported that depression and anxiety scores predicted smartphone addiction in a population of university students. Demirci et al. [8] also suggested that depression and anxiety were both associated with smartphone overuse among university students. In a systematic review, problematic smartphone use among adolescents was shown to be associated with increased odds of depression and anxiety [10]. In another systematic review, both depression and anxiety were related to problematic smartphone use, but with a medium effect size for depression and only a small effect size for anxiety [38]. However, Choi et al. [27] reported that anxiety was a risk factor for smartphone addiction, while depression was a protective factor.
One strength of the present study is that it included sleep patterns, sleep characteristics, and behavioral factors associated with daytime activity. In particular, the present study included an evaluation of sunlight exposure, which was shown to be associated with internet addiction. In addition, most of the questionnaires used in the study were simple and consisted of a relatively small number of items, allowing for excellent accessibility and convenient implementation. Nonetheless, this study had several limitations. First, all variables assessed in the study were acquired using self-reported questionnaires. Complementary parental reports or more objective evaluation methods, such as actigraphy, would have provided higher quality information, but such assessments are limited due to practical constraints in large numbers of subjects in a school setting. Second, due to the relatively rural location of Haman-gun in Korea, it is possible that the results were affected by regional bias. Therefore, future investigations in different cities and different populations are needed. Third, because this was a cross-sectional study, the causal effect of each factor could not be determined.
This study identified poor sleep quality, eveningness, and several other sleep-related patterns or behaviors as factors significantly associated with internet and smartphone addiction in adolescents in Korea. In addition, the results presented here show that anxiety could predict both internet and smartphone addiction. Additional studies should focus on establishing the role of interventions in these factors in preventing or alleviating internet and smartphone addiction in adolescents.
Notes
Funding Statement
This study was supported by a grant from the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HM15C1108).
The authors have no potential conflicts of interest to disclose.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Nuree Kang, So-Jin Lee, Bong-Jo Kim. Data curation: Nuree Kang, Bong-Jo Kim, Jae-Won Choi, Young-Ji Lee, Eunji Lim. Formal analysis: Nuree Kang, Bong-Jo Kim, Cheol-Soon Lee, Boseok Cha, So-Jin Lee, Dongyun Lee. Funding acquisition: Nuree Kang, Bong-Jo Kim. Investigation: Nuree Kang, So-Jin Lee, Dongyun Lee, Jiyeong Seo, Jae-Won Choi, Young-Ji Lee, Eunji Lim. Methodology: Bong-Jo Kim, Cheol-Soon Lee, Boseok Cha, So-Jin Lee. Project administration: Nuree Kang, Bong-Jo Kim, Cheol-Soon Lee, Boseok Cha, So-Jin Lee, Jiyeong Seo. Resources: Dongyun Lee, Jiyeong Seo, Jae-Won Choi, Young-Ji Lee, Eunji Lim. Software: Dongyun Lee, Jiyeong Seo, Jae-Won Choi, Young-Ji Lee, Eunji Lim. Supervision: Bong-Jo Kim, Cheol-Soon Lee, Boseok Cha, So-Jin Lee, Dongyun Lee. Validation: Bong-Jo Kim, Cheol-Soon Lee, Boseok Cha, So-Jin Lee, Dongyun Lee. Visualization: Dongyun Lee, Jiyeong Seo, Jae-Won Choi, Young-Ji Lee, Eunji Lim. Writing—original draft: Nuree Kang, Bong-Jo Kim, So-Jin Lee. Writing—review & editing: Nuree Kang, Bong-Jo Kim, Cheol-Soon Lee, Boseok Cha, So-Jin Lee, Dongyun Lee.