How Does Insomnia Affect Depression and Anxiety in Patients With Insomnia Disorder? A Symptom-Level Analysis
Article information
Abstract
Objective
This study investigated the specific symptoms of insomnia that are associated with depression and anxiety in patients with insomnia.
Methods
This study was a retrospective analysis of the data collected from 219 patients diagnosed with insomnia. The Insomnia Severity Index (ISI), Beck Depression Inventory-II (BDI-II), and Beck Anxiety Inventory (BAI) were used to assess the severity of symptoms of insomnia, depression, and anxiety. Spearman’s rank correlation and multiple linear regression analyses were used to analyze the data.
Results
All seven items of the ISI had a significant relationship with symptoms of depression and anxiety. Difficulty staying asleep and problems with sleep interfering with daily functioning had the greatest associations with the BDI-II total score. Problems with sleep interfering with daily functioning also had the highest correlation coefficient with the total BAI score. Multiple linear regression analysis showed that difficulty maintaining sleep and concerns about how others perceive sleep problems were significantly associated with depression. Difficulty falling asleep and problems with sleep interfering with daily functioning were significantly associated with anxiety.
Conclusion
This study suggests that specific symptoms of insomnia are associated with depression and anxiety in patients with insomnia. These findings may help clinicians to better understand the relationship between specific insomnia and affective symptoms and develop targeted treatment strategies for patients with insomnia.
INTRODUCTION
Insomnia is a subjective feeling of dissatisfaction with sleep and is very common, with a prevalence ranging from approximately 5% to 50% in adults; one-third of adults report at least one symptom of insomnia (i.e., difficulty initiating or maintaining sleep, non-restorative sleep) [1]. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), insomnia is a condition characterized by dissatisfaction with the quantity or quality of sleep and is associated with one or more of the following symptoms: 1) difficulty falling asleep, 2) waking up frequently or having difficulty falling back to sleep once awake, and 3) waking up in the morning and having difficulty getting back to sleep [2]. Additionally, insomnia is defined as a symptom of nonrestorative sleep and is associated with daytime consequences [3]. When a person has sleep difficulties of more than three nights per week for 3 months, a diagnosis of insomnia can be made [2]. These sleep difficulties occur even if there are sufficient sleep opportunities, and are associated with significant distress or impairment of daytime functions, including fatigue, energy loss, mood disorders, and cognitive impairment [4].
In the past, insomnia was characterized by its comorbidity with other psychological symptoms or disorders, and it was called secondary insomnia; however, recently, it has been understood as a comorbid condition of insomnia. Insomnia and affective symptoms, especially depression and anxiety, are closely correlated [5]. In patients with insomnia, severe levels of anxiety and depression are frequently observed, and the rates of accompanying depressive and anxiety symptoms were 9.82 and 17.53 times higher than people not having insomnia, respectively. In these cases, neither the severity of symptoms nor the prognosis was poor [6,7]. Patients with anxiety and depressive disorders had high rates of sleep disturbances [8]. In another study, chronic insomnia was found to be a risk factor for anxiety disorders [9]. Insomnia can be a risk factor for anxiety and depression [10].
As mentioned earlier, insomnia has several detailed symptoms, such as the inability to initiate sleep at bedtime, frequent awakenings, and early morning awakening [4]. In addition, patients with insomnia may worry about sleep problems, which can lead to affective symptoms such as anxiety or depression. Despite the variety of symptoms that constitute insomnia, the relationship between emotional disorders and insomnia has been studied primarily based on diagnosis. Therefore, this study analyzed the relationship between the individual symptoms of insomnia, depression, and anxiety.
METHODS
Study design and participants
This retrospective study was conducted at the Konkuk University Medical Center. Data were collected from the electronic medical records of patients diagnosed with insomnia based on the International Classification of Diseases, 10th Revision (ICD-10) criteria between January 2017 and January 2022 in the outpatient clinic of the Department of Psychiatry. Patients who failed to complete the baseline assessment questionnaires were excluded, and data from 219 patients were analyzed. As this study was retrospective, the need for informed consent was waived by the Institutional Review Board.
Measures
The Korean version of the Insomnia Severity Index (ISI) was used to assess insomnia symptoms [11]. The ISI is a self-reported questionnaire consisting of seven items. Each item measures the severity of different insomnia symptoms. It is as follows: 1a=difficulty falling asleep; 1b=difficulty staying asleep; 1c=problem of waking up early; 2=satisfaction/dissatisfaction with sleep pattern; 3=interference of sleep problems in daily functioning (e.g., daytime fatigue, mood, ability to function at work/daily chores, concentration, memory, mood, etc.); 4=impairment of quality of life noticeable to others; 5=worry/distress about sleep pattern. The severity of depressive and anxiety symptoms was assessed by the Korean version of the Beck Depression Inventory-II (BDI-II) [12] and the Beck Anxiety Inventory (BAI) [13], respectively.
Statistical analysis
The relationships between the detailed ISI questions and the BDI-II/BAI scores were analyzed using Pearson’s correlation and multiple linear regression analyses. In the regression analysis, the independent variables were the individual symptoms of insomnia and the seven items of the ISI, and the dependent variables were the total scores of the BDI-II and BAI. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS 17.0; SPSS Inc., Chicago, IL, USA).
RESULTS
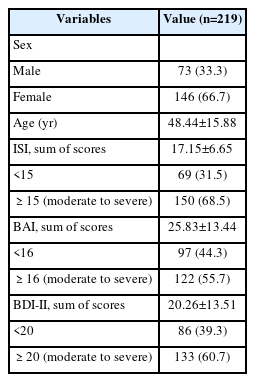
Table 1 presents the participants’ basic characteristics and variables. Among the participants, 33.3% were male and 66.7% were female (male=73, female=146), and the mean age was 48 years old (mean±standard deviation=48.44±15.88). In the case of insomnia, a score of 15 or more indicated moderate to severe symptoms based on the ISI score. In our sample, 68.5% of the participants had moderate-to-severe symptoms of insomnia. In the case of anxiety and depression, 55.7% and 60.7% of the participants showed moderate to severe symptoms, respectively.
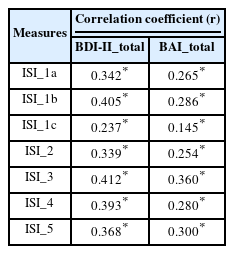
Table 2 shows the correlation coefficients between each ISI item and BDI-II and BAI total scores. The results showed that all seven items of the ISI had a significant relationship with symptoms of depression and anxiety (p<0.001). BDI-II had a slightly higher level of correlation with insomnia than BAI, and items 1b (difficulty staying asleep) and 3 (interference of sleep problems with daily functioning) showed a greater association with the BDI-II total score among the seven ISI items. In contrast, item 3 of the ISI showed the highest correlation with the total BAI score (r=0.360, p<0.001).
The results of the multiple linear regression analysis are presented in Tables 3 and 4. The symptoms of ISI items 1b and 4 were significantly associated with depression. In the case of items 1b (difficulty in maintaining sleep) and 4 (thoughts and concerns about how others perceive their sleep problems), the higher the score on these items, the higher the BDI-II total. In addition, younger female patients had the highest total scores in BDI-II and BAI among patients with insomnia. It was also found that the items 1a (having difficulty falling asleep) and 3 (interference of sleep problems in daily functioning) had significant effects on anxiety.
DISCUSSION
This study explored the symptoms of insomnia that cause depression and anxiety. In this study, anxiety and depressive symptoms were higher in younger female patients with insomnia. In addition, there was a significant correlation between the detailed items of the ISI and the BAI/BDI-II total scores. Failure to maintain sleep (item 1b) and disturbance in daytime functioning (item 3) were highly correlated with depressive symptoms, and item 3 showed the highest correlation with the BAI total score. In the regression analysis, inability to maintain sleep (item 1b) and worrying about showing one’s sleep problems to others (item 4) were significantly associated with depression, while the inability to fall asleep (item 1a) and interference with daytime functioning due to sleep problems (item 3) were significantly associated with anxiety.
By comparing the regression coefficients in each regression analysis, it was found that difficulty maintaining sleep, rather than difficulty falling asleep, was associated with higher symptoms of depression. This indicates that sleep maintenance has a greater effect on emotional symptoms than sleep initiation. Inability to maintain sleep caused depressive symptoms, which is consistent with the findings that poor sleep maintenance causes more symptoms of depression among postpartum women [14]. In addition, in other studies, insomnia and the decline in daytime function associated with insomnia can directly or indirectly cause a depressive episode; if this persists or becomes severe, it can lead to results that meet the diagnostic criteria for depression [15]. According to Suzuki et al. [16], sleep maintenance insomnia in patients with Parkinson’s was found to be significantly associated with symptoms of depression, which is partially consistent with the results of this study.
In the case of insomnia and anxiety, difficulty falling asleep increased symptoms of anxiety, which is consistent with the results of a study conducted in China, where a longer time for sleep initiation was associated with more symptoms of anxiety [17]. In a study of 2,393 elderly people aged 65 years or older, short sleep duration and daytime functioning problems were associated with anxiety [18]. The results of a study by Bragantini et al. [19], which found that individuals with severe anxiety complain of sleep-onset insomnia, support the results of this study.
Symptoms of depression and anxiety caused by insomnia are influenced by age and sex. Depression and anxiety were higher among the younger and female participants. This was consistent with the results of a study that investigated the bidirectional relationship between insomnia, depression, and anxiety among 625 participants who complained of strong anxiety where 62% were women, and of the 416 participants who complained of high levels of depression, 60% were female [7]. In general, depression/anxiety increases with age, and according to a cross-sectional study conducted in China, women experience more anxiety and depression than men, and patients with low education or low income experience higher levels of depression and anxiety, especially older adults [20]. However, the results of this study showed that it was different in insomnia patients, therefore, it can be speculated that younger people suffer more from insomnia.
In this study, we can find that insomnia can lead to affective symptoms. In a recent study on patients with insomnia during COVID-19, it was found that they were more vulnerable to exhibiting symptoms of anxiety and depression, and that pre-sleep arousal increases the risk of depression and anxiety [21]. In a study of 14,915 people from the UK, Germany, Italy, and Portugal, the proportion of patients with insomnia and daytime function decline was 19.1%, severity increased with age, and severe symptoms of insomnia lasting more than one year were predictors of multiple psychiatric disorders [22]. In another study of 1,420 adolescents aged 9–16 years, sleep problems increased the incidence of future generalized anxiety disorder (GAD), high GAD and symptoms of depression, and prevalence of oppositional defiant disorder [23]. This suggests that controlling sleep problems in adolescence is an opportunity to reduce the burden of mental illness in the future. Another interesting study in an older population found that depressive and anxiety disorders were more likely to occur with both shorter and longer sleep periods [24]. In addition, a study targeting postpartum women showed that poor sleep quality increases depression and anxiety [25], which is consistent with the results of other studies showing that poor sleep quality increases postnatal depression and anxiety [26,27].
One limitation of this study is that it was cross-sectional; therefore, it is difficult to conclude a causal relationship between insomnia and affective symptoms. Second, because this was a retrospective study, the influence of comorbid psychiatric disorders other than insomnia could not be excluded. Third, the relationship between affective symptoms and insomnia is generally bidirectional. For example, in several studies, sleep problems may be a prodromal symptom of depressive or anxiety disorders [28], while in another study, total sleep time was shortened by approximately 1 hour in patients with depressive and anxiety disorders [24]. Another study showed that sleep problems in adolescence were predictive of high levels of depression and anxiety, and vice versa [29]. Another cross-sectional study that investigated the role of anxiety and depression in causing insomnia in 3,600 respondents found that depression was more strongly associated with sleep initiation difficulty, and anxiety was strongly associated with sleep maintenance difficulty. These results suggest that the symptoms of depression and anxiety can cause insomnia [30]. However, only the effects of insomnia on depression and anxiety were investigated. In this study, which investigated the symptoms that cause depression and anxiety among insomnia symptoms in patients diagnosed with insomnia, it is possible to provide a treatment strategy that can prevent and treat the occurrence of depression and anxiety in insomnia patients.
Notes
Funding Statement
None
The authors have no potential conflicts of interest to disclose.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: all authors. Data curation: Gayoung Lee. Formal analysis: Gayoung Lee. Investigation: Hong Jun Jeon. Methodology: Gayoung Lee, Hong Jun Jeon. Project administration: Hong Jun Jeon. Supervision: Doo-Heum Park, Seung-Ho Ryu, Jee Hyun Ha, Hong Jun Jeon. Writing—original draft: Gayoung Lee. Writing—review & editing: Doo-Heum Park, Seung-Ho Ryu, Jee Hyun Ha, Hong Jun Jeon.