 |
 |
- Search
| Chronobiol Med > Volume 6(1); 2024 > Article |
|
Abstract
The excessive exposure of blue light, originated from electronic gadgets like smartphones, laptops, and tablets, may contribute to sleep problems. Long exposure to blue-wavelength light from these devices affects sleep by suppressing melatonin hormone and cause neurophysiologic consequences. This literature review highlights the most recent findings on the relationship between sleep disruption and blue light exposure among the high school and college student population. A variety of scientific studies have shown that blue light exposure, especially before bedtime, can create circadian disruptions and inhibit melatonin secretion in brain, which ultimately result in deteriorated sleep quality and duration. Sleep deprivation in duration and quality of sleep is reflected in negative effects on mood, learning memory, and academic performance of a student from middle school to college. In general, the accumulating evidence indicates that, to promote adolescent and young adult health, it is necessary to pay attention to the impacts of blue light exposure from modern technologies.
In recent decades, electronic devices including smartphones, tablets, and laptops have become ubiquitous in adolescent and young adult life [1]. A growing body of research recognizes that chronic exposure to blue light emitted from these device screens has the potential to significantly impact health and peace, particularly regarding the quantity and quality of sleep [2]. Blue light, encompassing wavelengths between 400–500 nm on the visible light spectrum, has been demonstrated to disrupt circadian rhythms and suppress production of the sleep hormone melatonin due to intrinsic photosensitive retinal ganglion cells that are sensitive to these wavelengths [3]. While some blue light exposure is necessary for circadian entrainment and melatonin regulation, excessive evening and nighttime blue light can shift the circadian timing and delay sleep onset [4]. Based on the evidence, the ubiquity of screen use may cause the high rates of inadequate and dysregulated sleep observed in student populations, which have previously been linked to effects on cognition, academic performance, mood regulation, attentiveness, and risk-taking decisions [5]. However, there has been little synthesis of the growing body of research specifically examining the biological impacts of blue light exposure on sleep quality, sleep duration, and downstream effects pertinent to adolescents and young adults engaged in secondary or post-secondary education. Therefore, this review aims to analyze and summarize the current literature surrounding the relationships between evening blue light exposure from electronic devices, disruption of healthy sleep cycles, and related outcomes for students.
The circadian system regulates nearly all 24-hour physiological processes in humans including the sleep-wake timing, hormone secretion, and body temperature regulation [6] (Figure 1). This intrinsic system synchronizes to the external light-dark cycle primarily through a subset of intrinsically photosensitive retinal ganglion cells (ipRGCs) containing the photopigment melanopsin [7]. These ipRGCs are maximally sensitive to blue light, peaking at wavelengths around 480 nm [8]. Through projections to the suprachiasmatic nucleus, the central circadian clock, and other brain regions, light detection by ipRGCs influences melatonin levels, sleep propensity, and circadian phase [9]. Data from a 2021 study on university students showed that just 2 hours of evening light exposure caused an average 1.1-hour circadian phase delay [10]. These effects can be greater in adolescents undergoing pubertal development in whom intrinsic circadian timing shifts naturally later. Survey-based research found that later school week bedtimes were predicted by increased evening screen use in students aged 13–18 years [11]. Longitudinal research tracking first-year college students (average age 18.8 years) linked the combination of irregular sleep schedules and late-night electronic device use to significant circadian delay and disrupted rhythm by the end of the fall academic term [12].
Melatonin is a neurohormone critical for regulating circadian rhythms and sleep-wake control. Under normal dark conditions at night, melatonin levels rise to peak concentration between 2–3 am, facilitating sleep initiation and quality [13]. Regulation of melatonin synthesis occurs through transcriptional activation of the arylalkylamine N-acetyltransferase (AA-NAT) and acetylserotonin O-methyltransferase (ASMT) enzymes. This is controlled by the suprachiasmatic nucleus of the hypothalamus and its inhibition by blue light exposure transduced via ipRGCs containing melanopsin photopigment [14]. Short wavelength blue light (460– 480 nm) has been shown to suppress nocturnal melatonin most substantially due to the peak ipRGC sensitivity occurring within this range [15] (Figure 2). Studies of college students have consistently demonstrated that blue light in the evenings causes both a reduction in melatonin levels and a phase delay in normal secretion patterns [16-18]. For example, following a 2-hour exposure to an LED tablet, students exhibited a 55% decrease in melatonin and an average melatonin onset delay of 1.5 hours compared to reading a printed book under low light [19]. Emerging research also indicates that genetic variations contribute to melatonin suppression vulnerability. A chronobiology study found individuals with PER3 polymorphisms linked to increased eveningness and delayed sleep phase disorder showed greater melatonin suppression to evening blue light relative to those without this trait [20]. Furthermore, variants in RORB which regulates melatonin biosynthetic enzyme transcription have been associated with dysfunction [21]. Individuals with risk genotypes exhibited blunted melatonin rhythms, likely exacerbated by evening blue light behaviors [22]. Genetic variations as mentioned affect vulnerability to melatonin disruption. Studies have uncovered polymorphisms in circadian clock genes like CRY1 [23], NPAS2 [24], and BMAL1 [25], and clock-controlled genes like PER3 [26] that modulate sensitivity of melatonin suppression following evening blue light. While direct evidence is limited thus far in humans, animal models provide insight into epigenetic changes that may underlie observed proteomic shifts. Mice exposed to dim blue light at night exhibited significant alterations in ocular DNA methylation patterns in phototransduction and circadian genes like Bmal1. Related chromatin remodeling changes in hippocampal neurons have also been shown in mice to affect learning, memory, and mood regulation potentially translating to humans [27].
Sleep quality refers to quantitative aspects like sleep efficiency, latency, awakenings, and self-reported feeling rested, whereas duration simply refers to total sleep time within a 24-hour period. High quality and sufficient sleep duration are essential for cognitive performance, academic achievement, mental health, and overall wellness [28]. However, pervasive evidence documents widespread prevalence of insufficient sleep and poor sleep quality among secondary school and university students associated with heavy electronic device use [29-31]. A meta-analysis reported students sleeping an average of approximately 7 hours per night with anywhere from 60%–80% indicating poor sleep quality linked to evening blue light exposure. Effects appear dose-dependent with over 4 hours of daily blue light device use predicting poorer sleep outcomes like low efficiency, daytime dysfunction, irregular timing, and latency issues [32]. Moreover, the persistent sleep deprivation and disruption during crucial academic years have downstream impacts. One study found that with each hour less of nightly sleep achieved by college students, the grade point average declined by nearly 0.07 on a 4.0 scale illustrating tangible effects [33]. Beyond academic marks, mood disorders, risk-taking behaviors, and drowsy-driving accidents increase with poor sleep [34]. Apart from behavioral effects, studies point to detrimental neurological and cognitive outcomes tied to chronic sleep restriction and irregular sleep patterns resulting from evening blue light exposure in adolescent students [35]. Magnetic resonance imaging scans have revealed reduced cortical thickness and volumes in frontal lobes essential to attention, memory, and complex processing after just a few nights of curtailed sleep [36]. Related studies on cognitive performance further demonstrate that one week of restricted sleep to 5 hours per night significantly slowed response times and impaired sustained attention compared to 9-hour sleep condition among teenagers [37]. Sleep deficits accumulate to a 17% and 13% respective reduction in critical thinking and working memory after only a few days based on standardized testing [38]. Additionally, learning and memory consolidation integral for academic content retention suffers, with data indicating a nearly 50% decrement in ability when students experience disrupted versus regular sleep [39].
The ubiquity of blue light-emitting electronic devices has led to chronic evening exposure that intrinsically disrupts circadian rhythms and suppresses the critical sleep hormone melatonin among adolescents and young adults. This environmental factor interacts with developmental changes of puberty delaying intrinsic sleep timing as well as societal pressures of early school start times and academic workload. The current body of evidence overviewed unambiguously links the blue light associated with LED device screens to detrimental impacts on sleep quality, sleep duration, and circadian regulation among secondary school and university students. Given the vulnerability of these populations due to neural maturation and lifestyle factors, the effects appear profound, contributing to highly prevalent insufficient and dysregulated sleep patterns. In turn, the acute cognitive and psychosocial correlates combined with long-term health outcomes attributable to poor sleep highlight this as a pressing issue requiring evidencebased solutions. While further research is needed, initial recommendations for students and institutions emphasize limiting evening blue light exposure, promoting better sleep hygiene practices, and exploring innovative filtering technologies. Addressing the impacts of blue light in youth will likely require a culture shift alongside science-guided interventions.
NOTES
Conflicts of Interest
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Figure 1.
The diagram depicts the human biological clock, with the inner circle illustrating melatonin concentration levels under typical blue light exposure conditions, while the outer circle represents melatonin secretion when subjected to heightened levels of blue light. An alteration in melatonin secretion occurs in response to excessive blue light exposure, consequently disrupting the balance of sleep patterns.
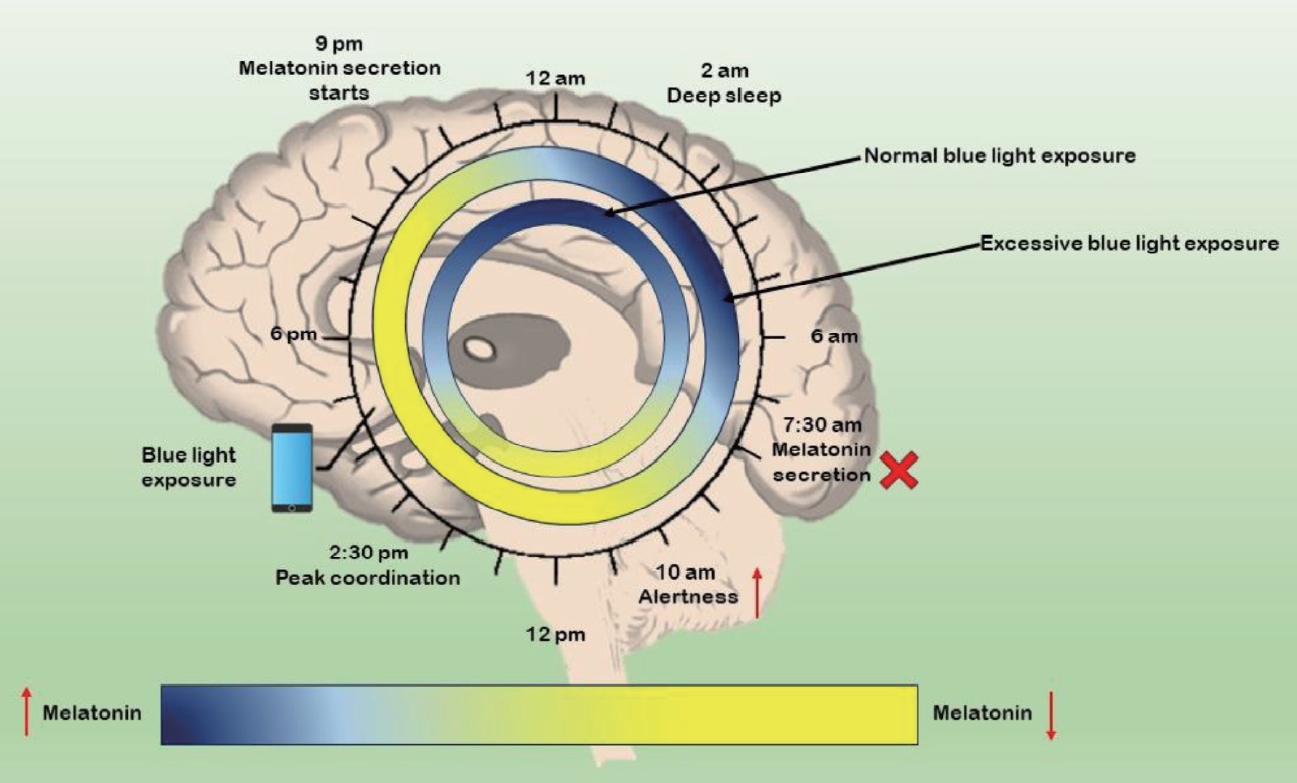
Figure 2.
When exposed to excessive blue light, intrinsically photosensitive retinal ganglion cells (ipRGCs) detect this light and transmit signals to the suprachiasmatic nucleus (SCN), subsequently initiating a negative feedback mechanism to the pineal gland, thereby inhibiting melatonin secretion. Conversely, in the absence of blue light, a positive feedback loop is triggered, leading to the secretion of melatonin. The presence of blue light activates the photoreception pathway, independent of the SCN, which includes the orexinergic pathway, dopamine-dependent pathway, and serotonin-dependent pathway. This activation results in an increase in sleep pressure and alertness, while simultaneously diminishing emotional regulation.

REFERENCES
1. Rashid SMM, Mawah J, Banik E, Akter Y, Deen JI, Jahan A, et al. Prevalence and impact of the use of electronic gadgets on the health of children in secondary schools in Bangladesh: a cross-sectional study. Health Sci Rep 2021;4:e388.




2. Silvani MI, Werder R, Perret C. The influence of blue light on sleep, performance and wellbeing in young adults: a systematic review. Front Physiol 2022;13:943108.



3. Tosini G, Ferguson I, Tsubota K. Effects of blue light on the circadian system and eye physiology. Mol Vis 2016;22:61–72.


4. Wahl S, Engelhardt M, Schaupp P, Lappe C, Ivanov IV. The inner clock-blue light sets the human rhythm. J Biophotonics 2019;12:e201900102.




5. Alshoaibi Y, Bafil W, Rahim M. The effect of screen use on sleep quality among adolescents in Riyadh, Saudi Arabia. J Family Med Prim Care 2023;12:1379–1388.



6. Reddy S, Reddy V, Sharma S. Physiology, circadian rhythm. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing, 2023. Available at: https://www.ncbi.nlm.nih.gov/books/NBK519507/. Accessed May 1, 2023.
7. Do MT, Yau KW. Intrinsically photosensitive retinal ganglion cells. Physiol Rev 2010;90:1547–1581.



8. Wong KY. A retinal ganglion cell that can signal irradiance continuously for 10 hours. J Neurosci 2012;32:11478–11485.



9. von Gall C. The effects of light and the circadian system on rhythmic brain function. Int J Mol Sci 2022;23:2778.



10. Pham HT, Chuang HL, Kuo CP, Yeh TP, Liao WC. Electronic device use before bedtime and sleep quality among university students. Healthcare (Basel) 2021;9:1091.



11. Alfonsi V, Scarpelli S, D’Atri A, Stella G, De Gennaro L. Later school start time: the impact of sleep on academic performance and health in the adolescent population. Int J Environ Res Public Health 2020;17:2574.



12. Phillips AJK, Clerx WM, O'Brien CS, Sano A, Barger LK, Picard RW, et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci Rep 2017;7:3216.




13. Zisapel N. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br J Pharmacol 2018;175:3190–3199.




14. Cipolla-Neto J, Amaral FGD. Melatonin as a hormone: new physiological and clinical insights. Endocr Rev 2018;39:990–1028.


15. Eo YJ, Choi SW, Kim C, Lee S, Yoon C, Kim DH, et al. Development and verification of a 480 nm blue light enhanced/reduced human-centric LED for light-induced melatonin concentration control. ACS Omega 2023;8:45547–45556.




16. Lee SI, Matsumori K, Nishimura K, Nishimura Y, Ikeda Y, Eto T, et al. Melatonin suppression and sleepiness in children exposed to blue-enriched white LED lighting at night. Physiol Rep 2018;6:e13942.




17. Shechter A, Kim EW, St-Onge MP, Westwood AJ. Blocking nocturnal blue light for insomnia: a randomized controlled trial. J Psychiatr Res 2018;96:196–202.



18. Higuchi S, Nagafuchi Y, Lee SI, Harada T. Influence of light at night on melatonin suppression in children. J Clin Endocrinol Metab 2014;99:3298–3303.


19. Schmid SR, Höhn C, Bothe K, Plamberger CP, Angerer M, Pletzer B, et al. How smart is it to go to bed with the phone? The impact of short-wavelength light and affective states on sleep and circadian rhythms. Clocks Sleep 2021;3:558–580.



20. Weiss C, Woods K, Filipowicz A, Ingram KK. Sleep quality, sleep structure, and PER3 genotype mediate chronotype effects on depressive symptoms in young adults. Front Psychol 2020;11:2028.



21. Ma H, Kang J, Fan W, He H, Huang F. ROR: nuclear receptor for melatonin or not? Molecules 2021;26:2693.



22. Figueiro MG, Wood B, Plitnick B, Rea MS. The impact of light from computer monitors on melatonin levels in college students. Neuro Endocrinol Lett 2011;32:158–163.

23. Yamanaka Y, Suzuki Y, Todo T, Honma K, Honma S. Loss of circadian rhythm and light-induced suppression of pineal melatonin levels in Cry1 and Cry2 double-deficient mice. Genes Cells 2010;15:1063–1071.


24. Haque R, Ali FG, Biscoglia R, Abey J, Weller J, Klein D, et al. CLOCK and NPAS2 have overlapping roles in the circadian oscillation of arylalkylamine N-acetyltransferase mRNA in chicken cone photoreceptors. J Neurochem 2010;113:1296–1306.



25. Hu Y, Yin J, Yang G. Melatonin upregulates BMAL1 to attenuate chronic sleep deprivation-related cognitive impairment by alleviating oxidative stress. Brain Behav 2023;13:e2836.

26. Charrier A, Olliac B, Roubertoux P, Tordjman S. Clock genes and altered sleep-wake rhythms: their role in the development of psychiatric disorders. Int J Mol Sci 2017;18:938.



27. Fonken LK, Aubrecht TG, Meléndez-Fernández OH, Weil ZM, Nelson RJ. Dim light at night disrupts molecular circadian rhythms and increases body weight. J Biol Rhythms 2013;28:262–271.




28. Nelson KL, Davis JE, Corbett CF. Sleep quality: an evolutionary concept analysis. Nurs Forum 2022;57:144–151.



29. Qanash S, Al-Husayni F, Falata H, Halawani O, Jahra E, Murshed B, et al. Effect of electronic device addiction on sleep quality and academic performance among health care students: cross-sectional study. JMIR Med Educ 2021;7:e25662.



30. Lin Y, Zhou X. Bedtime smartphone use and academic performance: a longitudinal analysis from the stressor-strain-outcome perspective. Comput Educ Open 2022;3:100110.

31. Liu B, Gao F, Zhang J, Zhou H, Sun N, Li L, et al. Sleep quality of students from elementary school to university: a cross-sectional study. Nat Sci Sleep 2020;12:855–864.


32. Jniene A, Errguig L, El Hangouche AJ, Rkain H, Aboudrar S, El Ftouh M, et al. Perception of sleep disturbances due to bedtime use of blue light-emitting devices and its impact on habits and sleep quality among young medical students. Biomed Res Int 2019;2019:7012350.




33. Creswell JD, Tumminia MJ, Price S, Sefidgar Y, Cohen S, Ren Y, et al. Nightly sleep duration predicts grade point average in the first year of college. Proc Natl Acad Sci U S A 2023;120:e2209123120.



34. Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep 2017;9:151–161.




35. Bacaro V, Andreose A, Grimaldi M, Natale V, Tonetti L, Crocetti E. The association between sleep patterns, educational identity, and school performance in adolescents. Brain Sci 2023;13:178.



36. Voldsbekk I, Bjørnerud A, Groote I, Zak N, Roelfs D, Maximov II, et al. Evidence for widespread alterations in cortical microstructure after 32h of sleep deprivation. Transl Psychiatry 2022;12:161.




37. Lo JC, Ong JL, Leong RL, Gooley JJ, Chee MW. Cognitive performance, sleepiness, and mood in partially sleep deprived adolescents: the need for sleep study. Sleep 2016;39:687–698.










