Association Between Obstructive Sleep Apnea (OSA) Severity and Optimal Continuous Positive Airway Pressure (CPAP); Do Severe OSA Patients Always Need High CPAP Pressure?
Article information
Abstract
Objective
Obstructive sleep apnea (OSA) is a prevalent sleep disorder associated with an increased risk of cardiovascular disease. Severity of OSA is assessed using the apnea-hypopnea index (AHI), but the optimal continuous positive airway pressure (CPAP) does not always correlate proportionally with AHI. This study aims to identify factors leading to the need for high CPAP pressure despite low AHI or vice versa.
Methods
The study includes 91 patients diagnosed with OSA through polysomnography. Participants undergoing CPAP titration were categorized in three groups based on AHI (30/h) and optimal CPAP pressure (10 cm H2O); low AHI and high CPAP pressure group (LH group), high AHI and low CPAP pressure group (HL group), direct proportion group (DP group). The Kruskal–Wallis nonparametric statistical test is used to identify significant differences between the three groups.
Results
Among the subjects, 78% were male, with no significant age or BMI differences between groups. There were 36 (39.6%) subjects with mild to moderate OSA and 55 (60.4%) subjects with severe OSA. The study revealed that patients requiring high CPAP pressure despite low AHI (LH group) had lower AHI, oxygen desaturation index, and various other parameters compared to other groups as expected. However, certain factors like the percentage of hypopnea in AHI, limb movement (LM) arousal index, and spontaneous arousal index were higher in the LH group.
Conclusion
Patients with mild to moderate OSA requiring high CPAP pressure are more likely associated with specific aspects such as hypopnea in AHI, LM arousal, and spontaneous arousal index, presenting unpredictable outcomes.
INTRODUCTION
Obstructive sleep apnea (OSA) is a common sleep disorder characterized by partial or complete obstruction of the upper airway, resulting in intermittent hypoxia. OSA is a complex condition that has a lasting impact on not only sleep quality but also quality of life, and is associated with diabetes, hypertension, stroke, coronary artery disease, and premature death [1,2]. While various surgical and non-surgical treatment options have been proposed, continuous positive airway pressure (CPAP) therapy has a proven role in reducing the adverse effects associated with OSA [3].
Optimal CPAP is defined as the minimum positive airway pressure that eliminates apneas, hypopneas, desaturation, snoring, and respiratory-related arousals, and optimal titration is most commonly achieved by inpatient polysomnography (PSG) [4]. More recently, automated positive airway pressure (APAP) machines have been introduced, allowing for unattended assessment at home [5].
Optimal CPAP levels are important, as lower than optimal CPAP levels can lead to insufficient treatment effectiveness or unintentional mask removal, while higher than optimal CPAP levels can lead to pressure intolerance and/or dry mouth [6].
CPAP has been successfully applied to many OSA patients, but factors that predict optimal positive airway pressure remain unclear [7]. Various prediction equations for optimal CPAP levels have been developed for different countries and populations from different geographic backgrounds, and their use could improve the success rate of manual titration and increase the convenience of treatments such as patient self-titration of CPAP or APAP [8]. However, they are rarely applied in clinical practice. The severity of OSA, defined by the apnea-hypopnea index (AHI), may predict the need for higher optimal CPAP, but there are few systematic studies evaluating whether severe OSA implies higher CPAP levels.
The optimal pressure of CPAP does not always increase proportionally with AHI. In general, higher AHI, body mass index (BMI), and Epworth Sleepiness Scale (ESS) scores tend to require higher CPAP pressure, but the positive predictive value is somewhat low, hovering around 30% [7,9-13]. The aim of this study was to identify several factors of patients requiring high CPAP pressure despite low AHI or conversely, requiring low CPAP pressure despite high AHI.
METHOD
Subjects
The medical records and nocturnal polysomnographic data of patients who visited the sleep clinic of Nowon Eulji Medical Center (Seoul, Korea) between January 2017 and May 2023 were retrospectively reviewed. We checked the data of patients who had both a baseline PSG and a PSG for CPAP titration, and found a total of 99 data. Among them, we found three cases where the same person had two PSGs for CPAP titration, and in these cases, we selected the one immediately after the baseline PSG for comparison. We also excluded two cases where the baseline PSG could not be confirmed and three cases where CPAP titration was not possible and APAP or bi-level positive airway pressure application was required. The subjects were divided into three groups based on AHI (30/h) and optimal CPAP pressure (10 cm H2O); low AHI and high CPAP pressure group (LH, AHI <30/h, CPAP pressure ≥10 cm H2O, n=15), high AHI and low CPAP pressure group (HL, AHI ≥30/h, CPAP pressure <10 cm H2O, n=17), direct proportion group (DP, n=59). This study was exempt from obtaining consent forms from the participants and approved by the Institutional Review Board of Eulji Hospital (EMCS 2023-11-012).
Polysomnography
All participants underwent nocturnal PSG (Medcare-Embla®, A10, S7000; Reykjavík, Iceland) consisting of an EEG (electrodes at F3, F4, C3, C4, O1, and O2, with A1 and A2 as reference sites), electrooculogram, submental and bilateral tibialis anterior electromyogram, and single-lead electrocardiogram. A nasal sensor to measure airflow, a respiratory inductance plethysmography band to evaluate thoracic and abdominal motion, and a finger pulse oximeter for monitoring oxygen saturation were also used. All data were assessed by qualified technicians and physicians according to the manual of the American Academy of Sleep Medicine (AASM) [14]. Sleep parameters including the AHI, PLMI, Oxygen saturation, time in bed, total sleep time, sleep efficiency, wake after sleep onset, sleep latency, REM latency, and percentage of N1, N2, N3, and REM sleep stage were calculated and recorded.
Self-reported questionnaire
All participants were asked to complete self-report questionnaires that captured demographic information (age, gender, weight, and height), medical history, and current medications (before nocturnal PSG). Korean version of the Pittsburgh Sleep Quality Index (PSQI-K) [15] was used to evaluate quality of sleep over the past month, and daytime sleepiness was measured using the Korean version of the ESS.
Statistical analysis
All statistical analyses were performed with SPSS software (version 23.0; IBM Corp., Armonk, NY, USA) and a p value <0.05 was considered statistically significant. Descriptive statistical analyses including the means and standard deviations were used to describe the average orientation and variability. The Kruskal–Wallis nonparametric statistical test was used to determine significant differences between the three groups, whereas the Mann– Whitney test was used to compare the subgroups.
RESULTS
Demographic and clinical characteristics
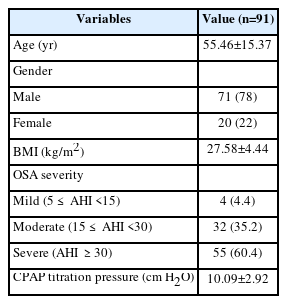
A total of 91 patients were analyzed, and this study mainly consisted of middle-aged men with severe OSA. The male ratio of the study subjects was 78%, and males accounted for a high proportion due to the nature of OSA. The mean age was 55.46±15.37 years, and the mean AHI was 42.68±22.40. There were 36 (39.6%) subjects with mild to moderate OSA and 55 (60.4%) subjects with severe OSA. The average BMI was 27.58±4.44 kg/m2, and the average CPAP titration pressure was 10.09±2.92 cm H2O. The general characteristics of this study’s participants are displayed in Table 1. And polysomnographic variables of all patients between baseline PSG and CPAP titration PSG are showed in Table 2.
Comparisons of PSG parameters between groups
Data from all study participants were categorized into three groups as presented in Figure 1; LH with low OSA severity but high CPAP pressure, HL with high OSA severity but low CPAP pressure, and a DP group in which the OSA severity and CPAP pressure are directly proportional.

Scatterplot of optimal CPAP pressure and OSA severity. OSA, obstructive sleep apnea; AHI, apnea-hypopnea index; CPAP, continuous positive airway pressure.
Mean age was not significantly different between the 3 groups (LH group, 58.7±10.5 years; HL group, 55.5±18.0 years; DP group, 54.6±15.7 years) and BMI did not differ significantly (LH group, 26.5±3.9 kg/m2; HL group, 26.5±3.7 kg/m2; DP group, 28.2±4.7 kg/m2). The general patient characteristics of 3 groups are displayed in Table 3.
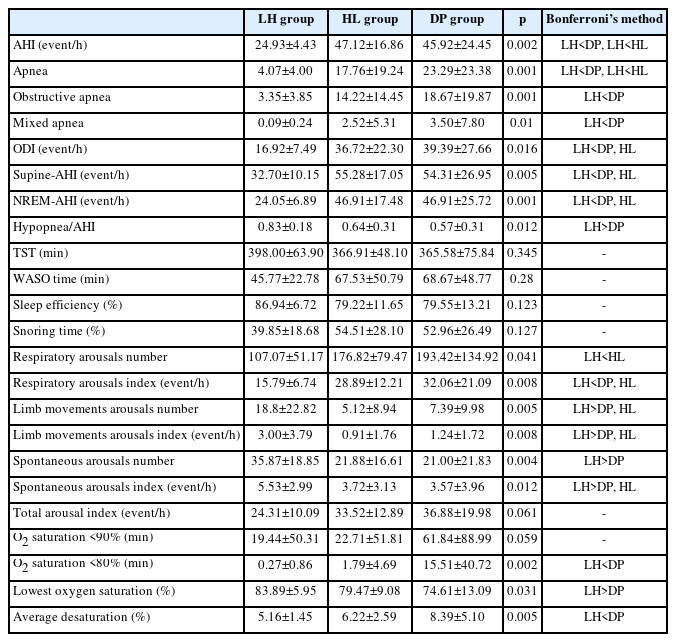
As expected, AHI, ODI, supine-AHI, NREM-AHI, apnea, obstructive apnea, and mixed apnea were lower in the LH group compared to the other groups. The time percentage of <80% O2 saturation (min) was also lower in the LH group compared to the control group, but the difference between the LH and HL groups was not significant. Lowest O2 saturation (%) was higher in LH group compared to control group, and average desaturation (%) was lower in LH group compared to control group. In addition, respiratory arousal number and index were also lower in the LH group compared to the HL group. However, the proportion of hypopnea in AHI was found to be higher in LH compared to the control group. Limb movement arousal and spontaneous arousal were also higher in the LH group compared to the HL group. It is possible that the proportion of hypopnea and limb movement are factors related to the need for high CPAP pressure even with low OSA severity (Table 4).
DISCUSSION
The severity of OSA is simply classified as AHI (mild, 5≤ AHI <15; moderate, 15≤ AHI <30; severe, AHI ≥30). However, there is a growing body of evidence that AHI alone is not sufficient to understand the complex and heterogeneous nature of OSA [16- 19]. It is also generally predicted that the more severe the OSA, the higher the CPAP level.
A previous study published in 2021 [20] evaluated the prevailing notion that patients with apnea-predominant OSA require higher therapeutic positive airway pressure (PAP) levels compared to patients with hypopnea-predominant OSA. The study concluded that there was no clinically significant difference between apnea-predominant and hypopnea-predominant patients, and that the percentage of obstructive apneas was not a strong predictor of therapeutic PAP levels. The study also concluded that the strongest predictor of PAP levels was AHI [20].
However, this study found that OSA severity and optimal CPAP level were not always proportional. The study identified factors affecting optimal CPAP in 91 OSA patients after integrating OSA severity, sleep-related symptoms, and several PSG variables. It also sought to identify factors associated with a group of patients with lower OSA severity who required higher optimal CPAP (LH group). In this study, there were no significant differences in age or BMI between the three groups. The AHI was lower in the LH group compared to the other groups, and the ODI, supine-AHI, NREM-AHI, apnea, obstructive apnea, and mixed apnea, time percentage of <80% O2 saturation (min), and average desaturation (%) were also lower. However, the proportion of hypopnea in AHI, limb movement arousal index, and spontaneous arousal index were higher in the LH group compared to the control group. In contrast to the findings of Yu et al. [20], this study found that PAP level and AHI were not proportional, suggesting that the percentage of apneas would affect PAP level. This suggests that the percentage of hypopnea and limb movement may be factors that affect CPAP pressure independent of OSA severity.
This study is significant because it suggests that hypopnea and arousal index may be predictors of optimal CPAP pressure, something that has not been addressed in previous studies. Utilizing factors that can predict optimal CPAP pressure could save time and money by allowing patients to set an effective pressure to improve OSA symptoms without the need for CPAP titration. We suggest that future studies investigate whether the patient characteristics and associated factors identified in this study can be applied to larger patient populations and can be used for cluster analysis of OSA.
Several limitations of our study should be mentioned. First, this study was conducted in Korean patients at a single center and is not ethnically diverse. Characteristics such as craniofacial morphology, nasal respiratory resistance, and obesity differ between Asian and non-Asian populations and may not be generalizable to other ethnicities [21-23]. Additionally, the higher proportion of male participants compared to females among the study subjects is another limitation. Second, we used only one titration night to determine optimal CPAP. Furthermore, one of the main limitations inherent to manual titration of optimal CPAP and a source of variability in the determination of optimal CPAP is found in the differences that may exist between the work accuracy of PSG technicians. However, all technicians performed CPAP titration according to AASM.
In conclusion, there are many factors to consider other than AHI as factors determining the optimal CPAP pressure. According to this study, patients with mild to moderate OSA who require high CPAP pressure are more likely to be associated with portion of hypopnea in AHI, LM arousal, and spontaneous arousal index, which is unpredictable result.
Notes
Eui-Joong Kim, a contributing editor of the Chronobiolgy in Medicine, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Ji Hyun Lee, Jae-won Choi. Data curation: Ji Hyun Lee, Jae-won Choi. Formal analysis: Ji Hyun Lee. Funding acquisition: all authors. Investigation: all authors. Methodology: Ji Hyun Lee. Project administration: Jae-won Choi. Resources: Jae-won Choi. Software: Ji Hyun Lee. Supervision: Jae-won Choi. Validation: Ji Hyun Lee, Jae-won Choi. Visualization: Ji Hyun Lee. Writing—original draft: Ji Hyun Lee, Jae-won Choi. Writing—review & editing: all authors.
Funding Statement
None
Acknowledgements
None