Incidence of Restless Legs Syndrome in Pakistan and Its Relationship With Depression, Gender, and Age: A Cross-Sectional Study
Article information
Abstract
Objective
Restless legs syndrome (RLS) is a neurological disorder known to cause an uncomfortable feeling in the legs, that is alleviated by movement and the symptoms are worse at night or in the evening This study aims to find out the prevalence of restless legs syndrome in Pakistan and to investigate whether it has any association with depression, gender or age.
Methods
In this cross-sectional study, a sample size of 377 was calculated using Raosoft. However, 400 participants were included after informed verbal consent, but after 20 dropouts, 380 sample size was finalized. The diagnosis of RLS was done by International Restless Legs Syndrome Study Group (IRLSSG) diagnostic criteria, the diagnosis of depression and its severity was checked by Becks Depression Inventory. A series of tests, namely, descriptive statistics, chi-square test, independent sample t-test, and one-way analysis of variance were calculated via SPSS Software version 27.
Results
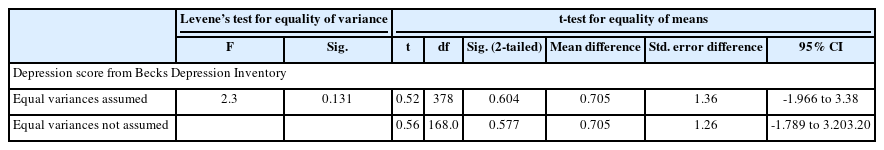
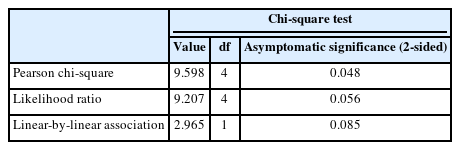
The prevalence of RLS in Pakistan is 23.7%. There was no difference in depression score with respect to RLS (F=0.270, p=0.604), and there was no difference in severity of depressive symptoms with respect to RLS (p=0.741). There was no difference in gender in prevalence of RLS (χ2=1.842, p=0.175). However, there is significant difference in RLS with respect to age (χ2=9.598, p=0.048).
Conclusion
RLS is quite common in Pakistan with a prevalence of 23.7%. However, the onset of RLS is unrelated to depression and gender, but the prevalence of RLS increases with age. Future studies should focus on investigating severity of RLS and ways to prevent it. It is relation with age can be studied further to help with the prognosis.
INTRODUCTION
Restless legs syndrome (RLS) is also known as Willis-Ekbom disease (WED). It is a common neurological or sensorimotor disorder that disturbs the quality of life and health of an individual. RLS is characterized by a strange feeling, often reported as paresthesia, particularly in the lower limb when the individual is at rest, accompanied by a strong urge to move the legs. The symptoms are prominent at night or evening, hence, it is also known to affect the quality of sleep and impairment of mental well-being [1,2]. The uncomfortable feeling is also referred to as dysesthesia (unpleasant or painful stimulus) or hyperesthesia (neurological condition known to have increased sensitivity to stimulus of touch/pain/temperature). Patient keeps moving at night to get rid of these sensations, as a result, the sleep quality is reduced [3]. RLS has been classified into two types: primary RLS and secondary RLS [4].
Primary RLS can be developed without a known cause, so it is often said to be idiopathic. The only reason that has been discovered is that it can be due to genetics [5] as 40% of RLS patients have a family history of this disease [4]. On the other hand, Secondary RLS develops as a result of certain pre-existing diseases like iron deficiency anemia, diabetes mellitus, end-stage renal disease, cirrhosis, hypertension, rheumatoid arthritis, multiple sclerosis, hypothyroidism, peripheral neuropathy, and Parkinson’s disease, with iron deficiency anemia, pregnancy, and end-stage renal disease being the most common reversible causes [4,6,7]. All these diseases are known to influence the central nervous system of the patient; hence, it is not incomprehensible that they can also be risk factors or causative factors for RLS. Furthermore, inflammatory reaction or immune responses are might also be involved in development of RLS [8]. The exact mechanism is unknown but it does suggest involvement of dopaminergic pathway as dopamine antagonist makes the symptoms worse while dopamine drugs improve them [9].
Despite RLS being common and having high prevalence, it is often undiagnosed in a lot of patients or even if it is diagnosed, it is undertreated [4]. The reason could be that most patients do not take these symptoms seriously and try to get by without seeking physician help.
The diagnosis of RLS is completely subjective and clinical. It is made based on symptoms described by the patient. A diagnostic criteria called URGE can be used [9]: U, urge to move the legs, associated with uncomfortable/unpleasant leg sensation; R, rest exasperate symptoms; G, gets better with movement; and E, worse in evening/night.
The treatment for RLS is only symptomatic. It helps relieve the uncomfortable sensation but there are no disease modifying drugs available. Dopaminergic drugs have been known to help alleviate symptoms [10]. Moreover, iron supplements, alpha-2-delta ligand (e.g., pregabalin, gabapentin), opioids, etc. are used [11]. Other than that there are a lot of non-pharmacological methods for treatment of RLS including yoga, physiotherapy, massage, exercise, and compression devices [12]. Non-pharmacological approach is for mild RLS, whereas for moderate to severe RLS, drugs are used [11].
Although there is a substantial amount of research about RLS/ WED, there are still some things related to the prevalence of this disease that are either not supported by research or are still ambiguous. Starting with the prevalence, it suggests that there is low prevalence in Asia, but the study also recommends more research because their results were limited to a region [11]. Contrary to the previous research, another research showed a higher prevalence in Korea, which is a country in Asia [13]. Pakistan is a country in South Asia, which was formed in 1947. With a population of over 240 million people [14], it is 5th most populated country in the world. It consists of people from various ethnicities and is a remarkably diverse country as it has 4 different provinces with 6 major ethnic groups and several small groups. In addition to that, theoretically, it is said that the prevalence of RLS increases with age [15] and more in young adults [3], but there is no research in the recent literature that provides any evidence to support this statement. A high prevalence of RLS has been associated with female gender as well [3,16], whereas, previous research stated that male gender plays a role in development of primary RLS [17]. Moreover, it has also been stated in previous literature that RLS correlates with depression. RLS patients have a higher rate of depression than people who do not have RLS [18]. However, another research reports that depression is not a risk factor for RLS or vice versa [19]. This research will shed more light on the previous controversial or ambiguous results of other research with the help of evidence and will try to identify the role of age, gender, and depression in the prevalence of restless legs syndrome. The objective of this study is to check the prevalence of RLS/WED in Pakistan and to check its association with depression, age, and gender.
METHODS
This is a cross-sectional study that was conducted in a tertiary educational institute after getting ethical approval from research ethics and support committee of the University of Management and Technology, Lahore. The data was collected from the students at the institute who ranged from first to fifth year, the faculty members and the questionnaire was also circulated on different social platforms to ensure variability in age groups and better generalizability. The sample size was calculated using Raosoft software [20] by keeping the margin of error at 5% with 95% confidence interval and it gave a suggested sample size of 377. However, a sample size of 400 participants was taken, but 3 of them missed a few questions in the questionnaire, and 17 participants did not return the forms. So, they were excluded, hence there were 20 dropouts. At the end, a total of 380 participants were included in this study who fulfilled the inclusion criteria. Informed verbal consent was taken from all the participants after explaining the rationale of the study. They were given a questionnaire that consisted of demographics (age, gender), clinical history, diagnostic criteria for restless leg syndrome, and depression rating scale. Age was divided into 5 age groups: 15–25, 26–35, 36–45, 46–55, and ≥56 years. The sampling was done through a convenient sampling method.
Diagnosis of RLS
The diagnosis of RLS was done via 2012 revised International Restless Legs Syndrome Study Group (IRLSSG) diagnostic criteria based on self-reported symptoms on the questionnaire. It includes: 1) an urge to move the legs with or without unpleasant sensation; 2) an urge to move the legs while the symptoms get worse at rest; 3) an urge to move the legs and symptoms getting better with movement; and 4) an urge to move the legs with unpleasant sensation getting worse at night or during the evening. These symptoms are not considered primary symptoms of another disease like positional discomfort, habitual leg tapping, limb edema, arthritis, myalgia, or leg cramps [21].
IRLSSG criteria have a sensitivity of 100% and specificity of 96.8% for correct diagnosis [22], and it is reported to be a highly accurate, valid, and reliable diagnostic tool [23].
Diagnosis for depression
The occurrence of depression was analyzed by a Beck Depression Inventory, which is based on 21 questions [24]. The score was calculated based on the participants’ responses indicating their level of depression. The interpretation is given as follows: 1–10, normal; 11–16, mood disturbance; 17–20, borderline clinical depression; 21–30, moderate depression; 31–40, severe depression; and over 41, extreme depression.
The limitation of this scale was that it was only for individuals above 13 years of age, so we had to modify our population accordingly.
The results for both RLS and depression score were calculated manually with correspondence to the given guideline of each questionnaire.
Inclusion and exclusion criteria
The inclusion criteria were: 1) age above 15 years; 2) people with no comorbidity diagnosed and healthy; 3) people who gave verbal consent; and 4) people who filled in the questionnaires completely. The exclusion criteria were: 1) age below 15 years; 2) pregnant or nursing women; 3) people who did not give consent; 4) people suffering from other sleep disorders; and 5) people who missed any part of the questionnaire.
Statistical analysis
The analysis was done using SPSS 27.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were run. Frequency was used to find out prevalence of RLS. To check the relation between RLS and depression severity, independent sample t-test and one-way analysis of variance (ANOVA) were performed. Chi-square test was done to analyze the relation between RLS and different age groups, and RLS with gender.
RESULT
This study includes 380 subjects that were analyzed after excluding the 20 dropouts. The prevalence of RLS in this group is 23.7% (Table 1).
Table 2 shows the relation between RLS positive individuals and gender (male and female) to test whether RLS is more prevalent in either of the genders. There was no difference between the genders with respect to prevalence of RLS (χ2=1.842, p=0.175) Hence, we were unable to reject the null hypothesis because prevalence of depression was not different between both groups in Table 3 (F=0.270, p=0.604), so the results were insignificant on both ANOVA and independent sample t-test (Table 4) as for the result to be significant, the p-value need to be less than 0.05. Another test was performed to check the relation between severity of depression and RLS. The results were insignificant too in Table 5 (p=0.741). On the other hand, there was a significant difference between distributions of RLS across different age groups represented by chi-square test (χ2=9.598, p=0.048) (Table 6). Our hypothesis about the relation between RLS and age was proved. The highest prevalence was seen in the age group 36–45 years old (53.8%), followed by 55 years or above at 50%, 26–35 years at 24.0%, and 15–25 years old at 22.5%.

The results of ANOVA between the participants RLS results and scores from Becks Depression Inventory
DISCUSSION
Restless legs syndrome was first described in the 1940s [1], but it has gained more attention in recent years. It was thought to be a rare disorder but over the course of years as more research was done on its prevalence, it was discovered that it is more common than we thought. The studies indicate that there is a high prevalence of RLS in general population of approximately 5%–10% [16]. There have been certain researches that are specific to regions that indicate different prevalence in different parts of the world like 7%–10% in Europe and America, 1%–7% in Asia, and 0.037% in Africa according to a study done in 2021 [11]. On the contrary, research of 2022 suggests a prevalence of 16.4% in adults of Germany and Switzerland, which are European countries. Likewise, a study in Korea on RLS suggests a 12% prevalence [13], which indicates a higher percentage in Asia, defying the percentage designated in the previous study [11]. There are a few studies done in Pakistan to check the prevalence of this disease but all of them are either on Pregnant women [25], diabetics [26], hemodialysis patients [27], or other patients having specific diseases. This research cannot be generalized. This study is the first to analyze the prevalence of RLS in general population of Pakistan and has revealed a prevalence of 23.7% in general population of Pakistan. Such a high percentage indicates that there are a lot of undiagnosed patients of RLS, and this number is much higher than the assumed percentage in Asia in the previous research.
Depression is defined as a serious and common disorder that negatively affects the thinking of a person along with how they feel about themselves and how they act [28]. Depression has been associated with RLS and is often recognized as a comorbidity [29]. A study in 2022 concluded that RLS patients had more severe depression and increased suicidal thoughts [18]. Whereas, another research indicates that depression is not a risk factor for RLS, yet they say that it increases the severity of depression [19]. There is an ambiguity in these results, which makes it unclear whether depression is associated with RLS or not, and whether RLS affects the severity of depressive symptoms. There is no study that compares the prevalence of depression between RLS positive and negative individuals. Therefore, this study is done to detect any correlation between depression and RLS. The result of this study confirms that depression is not linked with RLS, whatsoever. There was no difference in presence of depression among RLS positive and RLS negative participants (p=0.604, F=0.270) and when the severity of depression was compared, to check whether it is true that RLS adversely increases the severity of depression in depressed individuals, the results showed that the aforementioned statement is untrue (p=0.741). The studies mentioned above used DSM-5 diagnostic criteria for depression and it is not as accurate as Beck Depression Inventory for measurement of severity of depression because it is a more comprehensive diagnostic questionnaire. So, the reason this study does not agree with the previous study might be because Beck Depression Inventory is more accurate than the previous ones because it is more detailed and comprehensive with high precision. Also, the study design was to compare depression severity in a general population with or without RLS and there was no difference in the trend.
There is no earlier study that focuses on the onset of disease with respect to age. However, some mention that the earlier onset of RLS is before the age of 45 [30], the prevalence increases with age [15], while one study says that it is more common in younger adults [3]. Another study which was done to check the prevalence of depressive disorder in restless leg syndrome patients mentioned that there was no significant relation between RLS and age. However, their data was collected from an educational institute and they did not mention the range of participants with respect to the age, so the reason for insignificant result might be because the participants did not vary with respect to age [31]. None of the aforementioned studies were focusing on age as a variable so their suggestions were not supported with evidence or justifications. Whereas this study clearly indicates that the prevalence of RLS correlates with age. We obtained data from five different age groups i.e., 15–25, 26–35, 36–45, 46–55, and 56 years or above. We divided our participants into these age groups and the target was to collect data from diverse age groups. Hence, our results showed that RLS is most common in people who are 36–45 years old. Among the participants aged 36–45 years, 53% had RLS, followed by 50% of those aged 56 years or above. Additionally, 24% of 26–35-year-olds had RLS, which is almost half the rate of RLS in 36–45-year-olds, suggesting that the onset of RLS is twice as common in people in their 3rd and 4th decades of life compared to those who are younger. The lowest percentage was seen in the youngest age group of 15–25 years old at 22.5%, which is not a great difference from the older age group of 26–35 years old. Therefore, this study agrees with the statement that the early onset of RLS is more prevalent in people younger than 45 years. Also, the prevalence of RLS increases with advancing age (χ2=9.598, p=0.048).
RLS is believed to be genetic, but some sources mention that it is also related to gender. Subsequently, there is no research that takes gender as a variable and studies its relationship with RLS, independently. Nonetheless, the prevalence studies do categorize the participants into gender groups. Earlier studies have reported different results. Some say that both genders are equally affected [31], others mention that there is a higher prevalence of RLS in females (twice as much) [3,15]. Another study concludes that primary RLS is more common in males instead of females, while secondary was more common in females [17]. All these studies have conflicting results which makes the gender predisposition more ambiguous. Hence, to test it further, this study focused on gender as an individual variable and discovered that there is no significant correlation between gender and presence of RLS (χ2=1.842, p=0.175). There were a couple of limitations to this study listed as follows. First, most of the participants were from the 15–25 years age group, the participants were not equal with respect to the age categories. Second, the use of non-probability sampling or convenience sampling for selection of sample size. Third, the prevalence of RLS was not differentiated between Primary RLS and Secondary RLS as the symptoms of Secondary RLS improve if the underlying aggravating factor is treated.
Future recommendations
The next studies are recommended to study the relation of RLS with age further and check if severity of RLS is related to depression, age, gender, or any other variable. Since this study does not focus on severity of RLS, identifying the aggravating factors may improve the prognosis. Also, there is a need for awareness among society as this syndrome is severely underdiagnosed and often misdiagnosed. The patients suffering from RLS often have disturbed sleep patterns which adversely affect their lifestyle and productivity. Most of the time, they do not even know if they are suffering from any sort of disorder. Increased awareness will help these patients get the help they need and get rid of the symptoms improving overall physical health and better sleep outcomes.
Conclusion
RLS (or WED) is quite common in Pakistan, and the percentage is way higher than the percentage assumed in Asian population. However, RLS is unrelated to depression in any way. Neither does depression play a role in onset of RLS nor does presence of this syndrome increase the severity of depression in individuals. Moreover, there is no relation between RLS and gender. RLS equally affects both genders. Furthermore, the onset of RLS is related to the age of the individual. The prevalence of this disease increases with advancing age.
Notes
The authors have no potential conflicts of interest to disclose.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Riha Zahid, Muhammad Sundar Ali. Data curation: Riha Zahid. Formal analysis: Riha Zahid. Funding acquisition: Muhammad Sundar Ali. Investigation: Riha Zahid, Muhammad Sundar Ali. Methodology: Riha Zahid, Muhammad Sundar Ali. Project administration: Muhammad Sundar Ali. Resources: Riha Zahid. Software: Riha Zahid. Validation: Riha Zahid. Writing—original draft: Riha Zahid, Muhammad Sundar Ali. Writing—review & editing: Riha Zahid.
Funding Statement
None
Acknowledgements
None