Pulmonary Function and Effects of Body Position in Patients with Obstructive Sleep Apnea
Article information
Abstract
Objective
Obstructive sleep apnea (OSA) is known to be associated with upper airway collapse during sleep. However, OSA has also been suggested to have effects on the lower airway. This study examined the association between pulmonary function test (PFT) results during daytime and OSA according to the severity of OSA and presence of obesity. Changes in PFT results with body position (sitting vs. supine) were also analyzed.
Methods
A total of 46 patients who were diagnosed with OSA were included in this study. Patients were grouped according to the severity of OSA and presence of obesity.
Results
Obese, severe OSA patients tended to show poorer pulmonary function than non-obese, mild-to-moderate OSA patients. Forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC; sitting), peak expiratory flow (PEF; sitting), and forced expiratory flow during the middle half of the FVC (FEF25-75; supine) were significantly lower in the severe OSA group than the mild-to-moderate OSA group (p=0.020, p=0.044, and p=0.042, respectively). Positional change from sitting to the supine position significantly reduced pulmonary function in the total OSA patient population. The effect of body position on PFT results was greater in non-obese, mild-to-moderate OSA patients. FEF25-75 in the sitting position was still significantly related to the apnea-hypopnea index in OSA patients after adjusting for other factors (p=0.048).
Conclusion
This study indicated that relationships exist between lower airway function, body position, and OSA. The PFT is a simple test that can provide useful information about the upper and lower airways in OSA patients.
INTRODUCTION
Obstructive sleep apnea (OSA) is characterized by repetitive upper airway narrowing or collapse during sleep, which induces frequent arousal and oxygen desaturation [1,2]. OSA affects about 3.2–4.5% of the population of Korea and is associated with significant morbidity and mortality [3].
Polysomnography (PSG) is essential for diagnosis of OSA. However, PSG is expensive and requires specialized facilities and a significant amount of time to complete. Therefore, there have been attempts to develop other simple methods for diagnosing OSA, and to identify useful markers of the condition [4]. The negative expiratory pressure test, which consists of applying negative pressure during early expiration, has been suggested as one such method [4,5]. In addition, there have also been attempts to apply the results of the pulmonary function test (PFT) to the diagnosis and treatment of OSA [6-9].
The PFT is frequently performed in hospitals, and produces standardized results that are easy for clinicians to interpret. The PFT can also provide information on the lower respiratory tract, which may be involved in the pathogenesis of upper airway disease. Other studies also suggested that there are associations between OSA and intrathoracic airways [10-12].
In addition, there have been several reports regarding the effects of body position and obesity on PFT results [7,13,14]. In healthy subjects, PFT results are generally better in the sitting position than the supine position [15-17]. The sitting position was also reported to improve pharyngeal airway collapsibility in patients with OSA compared with the supine position [18]. However, there have been few studies focusing on the relationship between OSA and PFT results in both the sitting and supine positions; moreover, none of the existing studies are recent and they enrolled only small numbers of patients [7,8].
The present study was performed to examine the association between PFT results and OSA according to the severity of OSA and presence of obesity. Changes in PFT results with body position (sitting to supine) were also analyzed. We hypothesized that changes in PFT results with body position may be a useful indicator of OSA, especially in non-obese, non-severe OSA patients.
METHODS
Subjects
A total of 46 patients at Eunpyeong St. Mary’s Hospital, who were diagnosed with OSA using type 1 PSG, were included in this study. PSG was performed in the sleep laboratory of Eunpyeong St. Mary’s Hospital. Diagnosis and measurement of the severity of OSA were performed according to the definition of the American Academy of Sleep Medicine [1]. The inclusion criteria were 1) patients with OSA over 18 years of age and 2) patients who are able to undergo PFT in both the sitting and supine positions. The exclusion criteria were 1) pulmonary or infectious diseases; 2) any other medical condition that could affect pulmonary function; and 3) difficulties in sitting or lying in the supine position. Approval was obtained from the Institutional Review Board of Eunpyeong St. Mary’s Hospital (PC18EESI0060). All patients provided written informed consent prior to enrolment in the study.
Clinical measurements
Demographic data, including sex, age, body mass index (BMI), and smoking history were collected. Comorbidities, including diabetes, hypertension, congestive heart failure and cerebrovascular accidents, were also recorded. Apnea-hypopnea index (AHI), nadir peripheral capillary oxygen saturation (SpO2), oxygen desaturation index (ODI), and respiratory disturbance index (RDI) were determined based on the results of PSG.
Pulmonary function test in the sitting and supine positions
The PFTs were performed using a SensorMedics Vmax 229 instrument (Viasys Healthcare, Yorba Linda, CA, USA) during daytime. Before the PFT, each patient inhaled a short-acting bronchodilator (beta-2 agonist; salbutamol) four times within a period of 30 seconds. Although there is a low probability of air flow limitation reversibility in patients with normal spirometry [19], we nevertheless attempted to remove this confounding factor. The PFT was performed in the sitting position first, and then repeated 10 minutes later in the supine position.
Data analysis and statistics
Changes in PFT results with body position (sitting to supine) were analyzed in the total population. For subgroup analysis, the subjects were divided according to the severity of OSA and the presence of obesity. The mild-to-moderate OSA group (5≤AHI<30) was compared with the severe OSA group (AHI≥30). Obesity was defined as BMI ≥30 kg/m2. The mean and standard deviation were computed for normally distributed continuous variables, whereas the median and interquartile range (IQR, 25th to 75th percentile) were calculated for non-normally distributed continuous data. Categorical data are presented as numbers (%). The paired t-test was used to compare PFT results between the sitting and supine positions in the same patients. Student’s t-test was performed for normally distributed data, and the Mann–Whitney U-test for non-normally distributed data, to compare clinical data between subgroups. Categorical variables were compared using the chi-square and Fisher’s exact tests, as appropriate. Missing values were excluded from the analyses. Simple and multiple linear regression analyses were performed to identify the independent clinical predictors of AHI. Clinical parameters with a p-value <0.2 on simple regression analysis were included in multiple linear regression analysis. Statistical analyses were performed using R software (ver. 3.5.3; R Development Core Team, R Foundation for Statistical Computing, Vienna, Austria). In all analyses, p<0.05 was taken to indicate statistical significance.
RESULTS
Basic patient characteristics
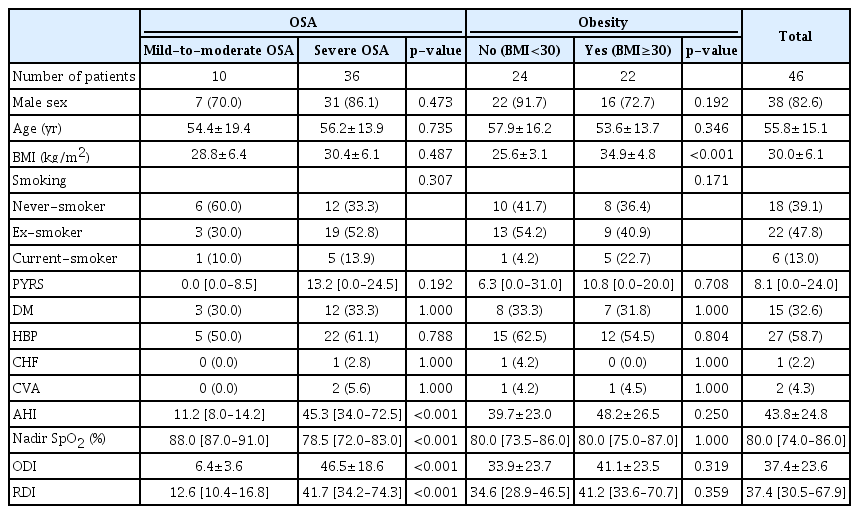
Table 1 lists the basic characteristics of the patients. Of the 46 patients with OSA, 82.6% were male. The mean age and BMI were 55.8±15.1 years and 30.0±6.1 kg/m2, respectively. The percentages of never-smokers, ex-smokers, and current smokers were 39.1%, 47.8%, and 13.0%, respectively. Hypertension was the most common comorbidity in the total study population (58.7%), followed by diabetes (32.6%), cerebrovascular accidents (4.3%), and congestive heart failure (2.2%). The PSG results revealed mean AHI, mean ODI, and median RDI values of 43.8±24.8, 37.4±23.6, and 37.4 (IQR: 30.5–67.9), respectively. The mean nadir SpO2 was 80.0 (IQR: 74.0–86.0).
We also performed subgroup analysis according to the severity of OSA and presence of obesity. Comparison of the mild-to-moderate OSA group with the severe OSA group indicated no significant differences in basic characteristics, except for parameters related to OSA (p<0.001 for AHI, nadir SpO2, ODI, and RDI). There were no significant differences between groups according to the presence of obesity, except for BMI (p<0.001).
Pulmonary function in the sitting and supine positions
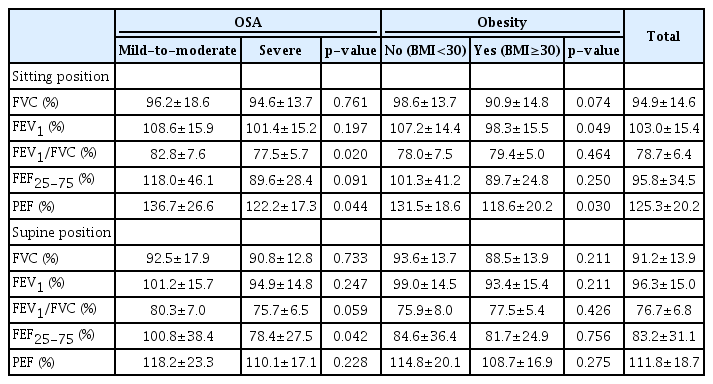
Among all OSA patients, there were significant differences in PFT results between the sitting and supine positions (Figure 1A). Compared with the sitting position, forced vital capacity (FVC, %), forced expiratory volume in 1 second (FEV1, %), FEV1/FVC (%), forced expiratory flow during the middle half of the FVC (FEF25-75, %), and peak expiratory flow (PEF, %) were all significantly lower in the supine position (p<0.001 for all comparisons).
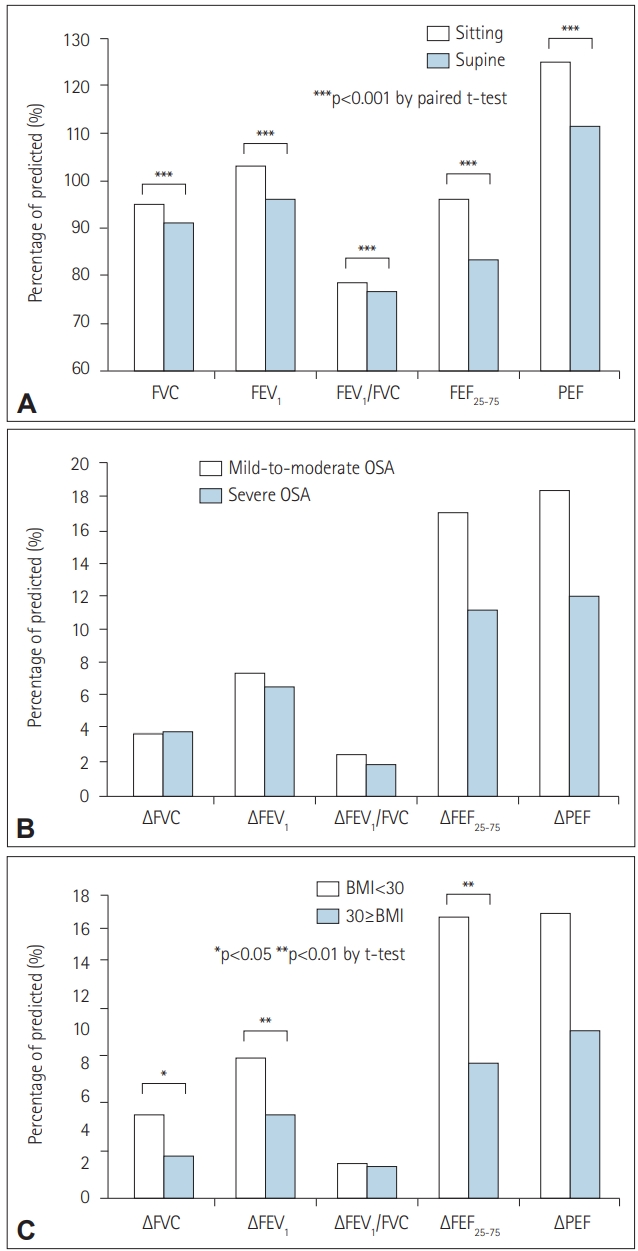
Change in pulmonary function test parameters in patients with OSA with change in body position (sitting vs. supine). (A) Pulmonary function in the sitting and supine positions. (B) Degree of pulmonary function change with change in body position in the mild-to-moderate OSA group and severe OSA group. (C) Degree of pulmonary function change with change in body position according to the presence of obesity. FVC: forced vital capacity, FEV1: forced expiratory volume in 1 second, FEF25-75: forced expiratory flow during the middle half of the FVC, PEF: peak expiratory flow.
In subgroup analysis according to the severity of OSA, the mild-to-moderate and severe OSA groups both showed significantly lower values in all PFT parameters in the supine position compared with the sitting position (Table 2). In addition, the severe OSA group generally showed lower values for all PFT parameters regardless of body position compared with the mild-tomoderate OSA group. Among the parameters, FEV1/FVC in the sitting position, PEF in the sitting position, and FEF25–75 in the supine position were significantly lower in the severe OSA group compared with the mild-to-moderate OSA group (P=0.020, p=0.044, and p=0.042, respectively).
Subgroup analysis based on the presence of obesity showed similar tendencies to subgroup analysis based on severity of OSA. The obesity and control groups both showed significantly lower values for all PFT parameters in the supine position compared with the sitting position. The obesity group tended to show lower values for the PFT parameters compared with the non-obese group. FEV1 and PEF in the sitting position were significantly different between the two groups (p=0.049 and p=0.030, respectively).
Degree of change in pulmonary function with change in body position according to the severity of OSA and obesity
The mild-to-moderate OSA group tended to show greater changes in pulmonary function parameters with change in body position compared with the severe OSA group (Figure 1B). However, the differences were not statistically significant.
The non-obese group showed greater changes in pulmonary function parameters with change in body position than the obese group (Figure 1C). The values of ∆FVC (%), ∆FEV1 (%), and ∆FEF25-75 (%) showed significant differences between the two groups (p=0.038, p=0.008, and p=0.007, respectively).
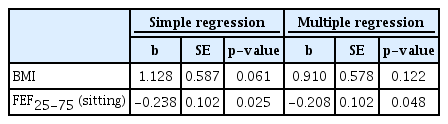
Clinical parameters associated with AHI in patients with OSA
On multiple regression analysis, FEF25-75 in the sitting position showed a significant association with AHI (p=0.048) (Table 3). The degree of pulmonary function change was not significantly associated with AHI. BMI was also not directly related to AHI.
DISCUSSION
In this study, we analyzed the daytime PFT results of OSA patients to determine the associations between OSA, pulmonary function, and body position. In the total OSA patient population, a significant decrease in pulmonary function was seen with a change from the sitting to the supine position; the decrease remained significant in subgroup analysis according to severity of OSA and presence of obesity. In addition, obese, severe OSA patients tended to show poor pulmonary function, and little change therein with a change from the sitting to the supine position, compared with non-obese, mild-to-moderate OSA patients. Finally, FEF25-75 in the sitting position was still significantly related to AHI after adjusting for other factors.
OSA is known to be associated with an increased likelihood of complete or partial upper airway collapse during sleep. However, OSA has also been suggested to have effects on the intrathoracic airways [10-12]. As well as the anatomical aspects, lower airway inflammation and oxidative stress may also impact pulmonary function [20]. Negative relationships were reported between the severity of OSA and PFT parameters, such as expiratory reserve volume [21], functional residual capacity [10], FEV1 [12,22], and FVC [12,23]. Although the absolute values of the PFT parameters in both of our groups were within the normal ranges, the severe OSA group tended to show poorer pulmonary function compared with the mild-to-moderate OSA group. Values of FEV1/ FVC in the sitting position, PEF in the sitting position, and FEF25-75 in the supine position were significantly different between the mild-to-moderate OSA and severe OSA groups. These results suggested the possibility of intrathoracic airflow disturbance in the severe OSA group compared with the mild-to-moderate OSA group. Reduction of pulmonary function according to the severity of OSA could be more meaningful in patients with respiratory disease, such as chronic obstructive pulmonary disease. The presence of OSA may exacerbate airway inflammation, and possibly lead to further deterioration of pulmonary function in patients with respiratory disease [24]. We also compared patients with OSA according to the presence of obesity, which is an important factor in OSA and respiratory function. Obese individuals are known to show reduced lung volume and capacity compared with individuals of normal weight [25]. The impact of obesity on lung function is multifactorial, encompassing both mechanical and inflammatory aspects [26]. Obese OSA patients tended to show poorer pulmonary function compared with non-obese OSA patients in the present study, which was consistent with a previous report [25]. There were no patients with obesity-hypoventilation syndrome (OHS) in our study population. However, we could not exclude a diagnosis of OHS due to a lack of daytime PaCO2 results.
According to the American Thoracic Society/European Respiratory Society (ATS/ERS) guidelines, the PFT may be performed in either the sitting or standing position, and the position should be recorded on the report [27]. There have been several reports regarding the effects of body position on lung function in healthy populations, obese subjects, asthma patients, and patients with spinal cord injury [13]. Pulmonary function was generally reported to be better in the sitting position compared with the supine position, except in some studies of patients with spinal cord injury.
Sleep position is an important factor in OSA, and patients are more likely to experience apneic events in the supine position [28]. Lung function was significantly better in the sitting position compared with the supine position in the total OSA population in the present study. The decrease in lung volume from the sitting position to the supine position may facilitate upper airway and intrathoracic airway collapse or closure, due to loss of caudal traction tension, and contribute to increased resistance in the airways [29]. Interestingly, the effect of position on pulmonary function was more prominent in our non-obese, mild-to-moderate OSA group than the obese, severe OSA group. These results suggest that the effect of position on the intrathoracic airway is greater in non-obese, mild-to-moderate OSA patients. In addition, obese, severe OSA patients already have lower pulmonary function compared with other OSA patient subgroups, even in the sitting position.
The relationship between decreased pulmonary function and severity of OSA must be interpreted carefully, because BMI is a strong confounding factor for this association [12]. In this study, FEF25-75 in the sitting position was the only factor significantly associated with AHI on multiple regression analysis. Although there has been some controversy regarding the association between pulmonary function and severity of OSA independent of obesity [23], our results were obtained after correction for BMI. Associations between lung volume and severity of OSA were also reported in studies matching subjects for BMI, or that adjusted for BMI [21,22]. FEF25-75 is considered an early marker of small airway disease [30]. The association between FEF25-75 and the value of AHI suggests the possibility of a relationship between OSA and lower airway pulmonary function. Several underlying mechanisms have been suggested, including airway inflammation and oxidative stress [20].
Our study had several limitations. First, the study population was small and a large proportion of patients were obese and had severe OSA. Therefore, we combined patients with mild or moderate OSA into one group. In addition, obesity was defined as BMI≥30 kg/m2. However, the non-obese group also showed a high mean BMI, of 25.6 kg/m2. Second, we attempted to control for important confounding factors, and patients with pulmonary disease or any other disease that can affect lung function were excluded. Patients who could not perform the test for any reason, and who were suspected to have pulmonary diseases based on spirometry results, were also excluded. Therefore, there was a possibility of selection bias in our study. Third, the PFT parameters were measured in the daytime, and were therefore not reflective of airflow during sleep, which was the main parameter of interest. Finally, we only performed spirometry, without examining lung volume or the diffusion capacity of the lungs for carbon monoxide. This study was performed to assess the intrathoracic airflow using a simple test. However, there were limitations in terms of understanding the lung mechanics in detail.
In conclusion, this study demonstrated the relationships of pulmonary function, body position, and OSA. Obese, severe OSA patients showed poorer pulmonary function, and also tended to show little change in PFT results with change in body position, compared with non-obese, mild-to-moderate OSA patients. FEF25-75 was correlated with AHI. Overall, the PFT can provide important information about upper and lower respiratory function in OSA patients. The PFT is easy to apply and may be useful as an early indicator of OSA.
Acknowledgements
This study was partly supported by Clinical Trials Center of Eunpyeong St. Mary’s Hospital.
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Sei Won Kim, Hyeon Hui Kang, Sang Haak Lee. Formal analysis: Sei Won Kim. Methodology: Sei Won Kim. Project administration: Sang Haak Lee. Resources: Sang Haak Lee. Writing—original draft: Sei Won Kim. Writing—review & editing: Sei Won Kim, Hyeon Hui Kang, Woo Ho Ban, Sang Haak Lee.