Restless Legs Syndrome Caused by Quetiapine
Article information
Abstract
In addition to patients presenting with primary restless legs syndrome (RLS), clinicians may also encounter patients presenting with drug-induced RLS. Drug-induced RLS is a commonly observed adverse event in patients receiving atypical antipsychotics (AAP). The individual AAPs have been shown to induce RLS at varying frequencies. In particular, olanzapine and quetiapine have been reported to induce RLS at higher rate than do the other AAPs. Considering quetiapine’s low affinity for the dopamine receptor, AAP-induced RLS cannot be attributed to the degree of dopamine blockade alone. Observations from previous pharmacokinetic studies indicating that quetiapine exhibits transiently high D2 occupancy when initially administered could offer an explanation for this high rate of RLS induction. Several additional reports have indicated that the symptoms of RLS may be exacerbated by administration of anti-histaminic drugs, which is of interest in the context of quetiapine’s high affinity for the H1 receptor. Still, the exact mechanism by which AAPs induce RLS remains unclear. This article will review the current clinical evidence regarding quetiapine-induced RLS.
INTRODUCTION
While in clinical practice, clinicians may encounter patients presenting with drug-induced restless legs syndrome (RLS) in addition to those presenting with primary RLS. RLS is particularly and commonly observed in patients receiving atypical antipsychotics (AAP), which as a class are known to exert their clinical effect through antagonism of the dopamine receptor. However, the probability at which administration of the individual AAPs may induce RLS has been seen to be inconsistent. Quetiapine and olanzapine in particular have been observed to be potent inducers of RLS. As such, it is difficult to ascribe AAP-induced RLS to dopamine antagonism alone when considering quetiapine’s low affinity for the dopamine receptor.
PATHOPHYSIOLOGY OF QUETIAPINEINDUCED RLS
RLS has previously been associated with iron deficiency, pregnancy, kidney disease, and rheumatoid disease as well as disruption of dopamine and histamine signaling [1]. Additionally, associations between drug-induced RLS and dopamine (D2) receptor blockers, histamine receptor blockers, antidepressants, lithium, and caffeine have been described [2].
Dopamine and quetiapine-induced RLS
The mechanism by which AAPs may induce RLS remains unclear. The primary mechanism has been suspected to be related to a disruption in dopaminergic signaling [3]. However, by this reasoning, quetiapine would be expected to induce RLS at a lower rate than that of olanzapine and risperidone owing to its lesser occupancy of the D2 receptor [3]. This supposition is further questioned by additional observations that quetiapine only loosely binds to the D2 receptor and readily dissociates from it [4]. To that end, other studies have even shown that quetiapine induces akathisia at a similar rate to placebo [5,6]. Investigators have hypothesized that quetiapine’s tendency to transiently bind D2 at high occupancy [7] when initially administered could be a contributing factor to the high rate of RLS reported during its use [8]. However evidence in support of this mechanism remains inconclusive.
Histamine and quetiapine-induced RLS
Quetiapine has been found to display a high affinity for the H1 receptor, and several reports have described exacerbation of RLS symptoms on administration of antihistaminic medication [9]. In addition, some investigators have reported that administration of antihistamines, antidepressants, antipsychotics, and antiemetics may increase the risk of RLS in patients with end stage renal disease [10]. However, at the same time, a recent study has revealed the possible involvement of a striatal histamine mechanism in the pathogenesis of iron-deficiency anemia-induced RLS, and that histamine H3R antagonism may be efficacious in its management [11]. Therefore further study of the relationship between histamine and RLS continues to be warranted.
Iron deficiency and quetiapine-induced RLS
Other studies have suggested involvement of iron dysregulation in the pathogenesis of quetiapine-induced RLS [9]. Iron deficiency has been shown to be a common cause of secondary RLS. Insufficient supply leads to a disruption in dopamine synthesis, increasing variation in the diurnal cycle [9]. An underlying iron deficiency may increase susceptibility to RLS, and supplementation could possibly mitigate symptom severity [12]. Thus, clinicians may benefit from remaining cognizant of a patient’s iron status when management has been complicated by the presence of RLS.
DIFFERENCE BETWEEN ANTIPSYCHOTICINDUCED AKATHISIA AND ANTIPSYCHOTIC-INDUCED RLS
Because severe cases of antipsychotic-induced RLS that have lost circadian variation may be challenging to distinguish from those of akathisia, discerning between the two is sometimes difficult [13]. The symptoms of antipsychotic-induced RLS increase during the night and the discomfort is localized to the lower extremities [1,14]. However, patients may describe either condition as an inner restlessness. Given this, RLS should be considered with a higher index of suspicion than akathisia in patients managed on quetiapine, as quetiapine is much more likely to induce the former rather than the latter [3,4].
CASE SERIES OF QUETIAPINE-INDUCED RLS
A literature search was conducted using the term ‘quetiapine’ OR ‘restless legs syndrome’, OR ‘RLS’ in Medline, EMBASE, and PsycINFO. Table 1 summarizes the results of that search limited to case reports of quetiapine-induced RLS [8,15-24]. Dosages of quetiapine administered in the studies ranged from 25 mg to 600 mg. Low as well as high dosages of quetiapine were seen to be capable of inducing RLS.
A total of 22 cases of quetiapine-induced RLS have been reported. Among them, 17 patients were females, and 5 patients were males. These results were consistent with previous studies that reported a higher prevalence of primary RLS in women compared to men [25]. However, the small sample size limits the statistical power of this observation.
Mean age of all patients was 46.5 years. Mean ages of the males and females were 52.6 years and 44.7 years, respectively. A majority of the patients carried psychiatric diagnoses (bipolar disorder, n=10; major depressive disorder, n=10; schizoaffective disorder, n=1; borderline personality disorder, n=1). Investigators have hypothesized that depression and RLS could synergistically increase susceptibility to RLS [26]. And although strong evidence is lacking, the effects of concomitant administration of other medications such as antidepressants cannot be discounted. A proposed mechanism for this phenomenon involves inhibition of dopaminergic signaling by selective serotonin reuptake inhibitors [26]. Fourteen patients were being managed on a combination of quetiapine and an antidepressant (Table 1). Thus, the effects of antidepressant administration as well as quetiapine administration alone, and that of a possible interaction between an antidepressant and quetiapine on the incidence of RLS could not be individually assessed in those patients. However, in four of the other patients it was possible that quetiapine alone was responsible for the onset of RLS. In one of those patients, a single low dose (100 mg) of quetiapine is believed to have induced RLS. However, at the same time, there has been another report submitted to the literature that documents the mitigation of clonazepam-refractory RLS in a female patient after a single dose of low-dose (25–50 mg) quetiapine [27]. Thus, continued investigation of this matter is required.
The patients were on a wide variety of medications (venlafaxine, n=4; amitryptiline, n=2; mirtazapine, n=2; duloxetine, n=2; escitalopram, n=2; citalopram, n=1; fluoxetine, n=1; trazodone, n=1; sertraline, n=1; bupropion, n=1). Four patients were on oxcarbamazepine and two patients were on valproate.
TREATMENT OF QUETIAPINE-INDUCED RLS
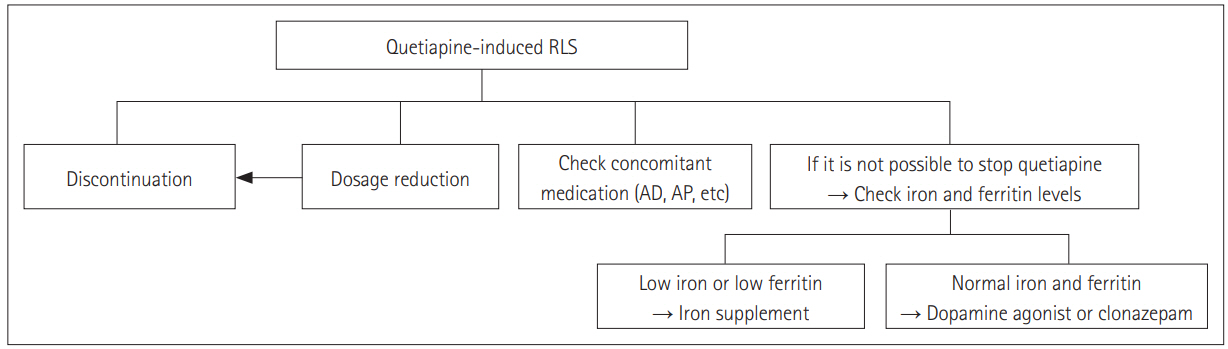
Quetiapine-induced RLS is often readily identified, and symptoms usually improve on termination of quetiapine or a dosage reduction (Figure 1) [8,22]. In times when taking the patient off of quetiapine may be disadvantageous, the addition of a dopamine agonist such as ropinirole or pramipexole, and possibly clonazepam, may serve to mitigate RLS symptoms (Figure 1) [8,18,22]. In specific cases, determining serum iron and ferritin levels may be of benefit, as if there were to be a concurrent iron deficiency in a patient with quetiapine-induced RLS, iron supplementation may mitigate symptoms like other secondary RLS. Although there has been no report on iron supplement in a patient with quetiapine-induced RLS, some investigators reported the improvement in antipsychotic-induced akathisia with iron supplement in a patient with iron deficiency [28].
CONCLUSIONS
Quetiapine-induced RLS is more commonly encountered than that caused by other AAPs [8]. Although the primary pathophysiology has yet to be clearly identified, clinicians should be aware of this adverse effect of quetiapine. Further studies on this matter are necessary.
Acknowledgements
None
Notes
The author has no potential conflicts of interest to disclose.