Light Therapy in Mood Disorders: A Brief History with Physiological Insights
Article information
Abstract
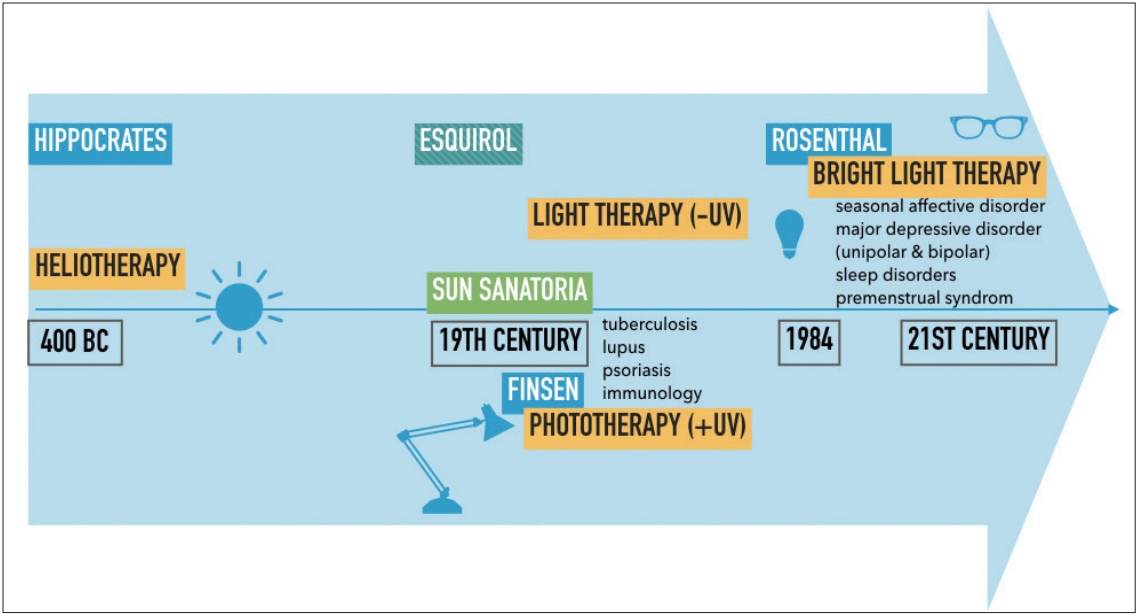
The mother of today’s Bright Light Therapy (BLT), Heliotherapy, has been the longest used form of phototherapy and the only one until the mid-nineteenth century. Sun therapies were applied in ancient Chinese, Hindu and Egyptian medicine over 15 centuries BC. Since the invention of the electric light bulb and the progress of medicine, heliotherapy shifted to: ultra-violet (UV) phototherapy, which is still used today in dermatology, immunology or neonatology; and to light therapy (UV filtered light) in the treatment of neurological, endocrinological and psychiatric affections. BLT is today the gold standard treatment of the Seasonal Affective Disorder, and is recommended in various others affective disorders. Recent findings as the Zeitgeber Theory involving the Central Biological Clock, and the implication of photo transductor melanopsin in the regulation of the circadian clock are guiding chrono-biologists to understand the physiological insights underlying BLT’s action on affective disorders. Those researches combined with ongoing clinical trials could guide us toward an optimal use in mood disorders of this millennial therapeutic resource.
INTRODUCTION
The relationship between mood and light changes has been described since Antiquity, and has shown growing interest since the publication of a series of cases of patients successfully treated for winter depression by Rosenthal and his colleagues [1] in 1984. Light therapy is both an old and a new treatment, as light therapy benefited from new insights and extensive indications for mood disorders ranging from seasonal affective disorders to non-seasonal unipolar or bipolar depressions [2]. This particular interest is also being re-emerging thanks to pre-clinical and clinical evidence showing alterations of the biological clock and light-signalling systems in mood disorders [3]. We were therefore interested in the history of the use of light for medical purposes that led to its current use in the more precise indication of mood disorders.
METHODS
We conducted a critical and narrative review of the scientific literature, searching for relevant national and international articles that had an interest in light treatment for mood disorders. The publications were obtained from the Medline, Google Scholar and SUDOC electronic database. The literature search was performed using the keywords: (“bipolar disorder” OR “mood” OR “depression” OR “Depressive disorder”) AND (“light” OR “bright light therapy” OR “phototherapy” OR “heliotherapy”). The search was updated until September 1st, 2018. Only articles written in English or French were considered as eligible. We included books, comments, original studies, reviews, case series and studies, that assessed light as a treatment for mood disorders.
FROM HIPPOCRATES’ HELIOTHERAPY TO ROSENTHAL’S LIGHT THERAPY
Ever since Antiquity
Humans from all latitudes, ever since Antiquity, have always worshiped the Sun which has been repeatedly considered as a god all around the world: Ra in Egypt, Helios in Greece, Inti for the Incas. The relationship between mood disorders and the light changes between seasons is described for the first time by Wong Tai over 4700 BC [2]. In Ancient Greece, it is reported that Asclepius, god of Medicine, whom Hippocrates was believed to be the descendant of, had directly inherited the Sun from Helios and Light from Apollo. This legacy is found in the first sentence of the Hippocratic Oath: “I swear by Apollo, doctor, by Asclepius, by Hygiea and Panacea…” Hippocrates indeed wrote the first texts about therapeutic benefits of sunlight on mood and mental health and named this therapy: Heliotherapy. The first sentence of his famous book On Airs, Waters, Places [4] (about 400 BC), was: Whoever wishes to investigate medicine properly should proceed thus: in the first place to consider the seasons of the year, and what effects each of them produces for they are not all alike, but differ much from themselves in regard to their changes. […] In the same manner, when one comes into a city to which he is a stranger, he ought to consider its situation, how it lies as to the winds and the rising of the sun; for its influence is not the same whether it lies to the north or the south, to the rising or to the setting sun. His writings were then to be paraphrased, analyzed and developed by Roman doctors such as Galen, or Arab doctors such as Avicenna. They emphasized the possible negative consequences of insufficient light [5]. This idea will then be revisited by popular cultures as illustrated by the Czech proverb: “Where the sun does not shine, goes the doctor” or this Persian proverb saying: “When you shut out the sun from coming through the window, the doctor comes at the door.”
Not far from there, Aretaeus of Cappadocia (II–I century BC) will be the first to consider melancholy and mania as part of the same nosological entity. He is therefore the first to conceptualize what is now called bipolar disorder [6]. Aretaeus of Cappadocia said about light effects on mood that “Lethargics are to be laid in the light and exposed to the rays of the sun, for the disease is gloom.” [7].
At the beginning of the 19th century
The first application of light therapy in modern psychiatry can be identified in the Œuvre pratique by Jean-Etienne Dominique Esquirol, Pinel’s pupil, who wanted his fellows to completely rethink the asylum in its location, orientation and architecture. For Esquirol, “a psychiatric hospital is an instrument of healing” if its premises are both pleasant and hygienic [8]. It started in 1818 with his memoir about insane asylums, presented to the French Ministry of the Interior (equivalent to the Home Secretary of the United Kingdom). He then published a second memoir entitled Des établissements d’aliénés (About Insane Asylums) [9], extended with new observations he made in France and abroad. He visited hospitals in Belgium and Italy, and studied the architectural designs, the description and the regulations of the main mental houses in Europe and America. He then wrote: 『I saw them, naked, covered in rags, having only straws to protect themselves from the cold dampness of the pavement on which they laid. I saw them grossly fed, deprived from air to breathe and from water to quench their thirst. […] I saw them in tiny, dirty, filthy, airless rooms, without light, enchained in dens where one would fear to enclose ferocious beasts. […] This is what I have seen almost everywhere in France, this is how the insane are treated almost everywhere in Europe』 [10].
He guided the construction of many French hospitals such as in Marseille, Le Mans, Rouen, Montpellier, Nantes and his major work: The Royal House of Charenton. He led the architect ÉmileJacques Gilbert in the design of what was then called “The Asylum of Charenton,” as he states in Mental maladies: a Treatise on insanity [8]: 『The courts of the building must be placed east and west, and if the construction is well understood, the entrance to the building will be north because the galleries where the patients walk should front the south.』 This architecture is still found today on the Esquirol Site of the National Hospitals of Saint-Maurice. As such, Esquirol promoted the central place of light in the architecture of Asylum and so in the treatment of patients.
During the same period, exposure to the sun was indicated as a treatment for tuberculosis or for skin conditions such as lupus and eczema. The therapeutic virtues of the sun were recognized on the psychiatric, cutaneous and immunological fields. Sanatoria were built to benefit from natural sunlight during the late 19th century to fight the tuberculosis epidemic. Sanatoria were founded to provide patients with good food, fresh air and sunlight exposure. Arnold Rikli, Oskar Bernhard and August Rollier were the firsts to seriously use sunlight (helio) therapy in the treatment of tuberculosis [11,12]. Rikli applied the principle “Water is good, the air is better, and most of all the sunlight.” Bernhard promoted heliotherapy in the beginning of 1899 at a private clinic in St. Moritz, Switzerland, while Rollier applied climatic treatment in combination with phototherapy for the treatment of tuberculosis of the bone, beginning in 1903 at a sanatorium in Leysin, Switzerland (Figure 1). Heliotherapy was considered to be more effective in treating tuberculosis than the chemotherapy available back then. The growing interest in those Sun Sanatoria coincided with an increased appreciation of the association of sunlight and health among the general public. The effects of sunlight on the skin was to induce the production of nitric oxide and vitamin [11]. Vitamin D is responsible for immune system functions and multiple studies have found an association between tuberculosis immunity and high vitamin D levels. Therefore, it is understandable that providing tuberculosis patients with sunlight may have boosted their immune system and aided them in the fight against tuberculosis [11,13].
In 1890 the Danish physicist Niels Ryberg Finsen developed the first carbon arc lamp (Figure 2), producing ultra-violet (UV) radiation and was awarded the Nobel Prize of Medicine in 1903 for his work [13]. This marks the beginning of modern phototherapy, which was used during this period to treat the Lupus vulgaris.
Since then, ancient heliotherapy was thus separated into two distinct medical branches: 1) phototherapy, which uses natural or artificial UV rays A and B (then associated with exogenous photosensitive molecules in dynamic phototherapy), and 2) light therapy, which uses natural—then artificial—light spectrum, without UV rays (UV filter) to treat depressive syndromes (amongst other syndromes) by a direct effect on the central nervous and hormonal systems and indirect effects on the biological clock [14].
Towards modern light therapy
As far as the field of psychiatry is concerned, it was not until the beginning of the 1980s that Norman Rosenthal, a South African doctor practicing in Washington, got interested in light therapy, observing at his own expense that he was feeling depressed at the arrival of autumn and then feeling a mood improvement in early spring. In 1984, with the help of his group of researchers at the National Institute of Mental Health in the United States, he published the first scientific description of the Seasonal Affective Disorder, or SAD [1]. Most frequently, patients experience depressive symptoms during fall and winter, with full remission to euthymia or switch into (hypo)mania during spring and summer [15]. Rosenthal presented the first case series describing the antidepressant effect of light on these patients suffering from SAD [1]. The first devices used in the eighties were large boxes equipped with powerful light bulbs (Figure 3), which will later be called light therapy lamps.
Nowadays
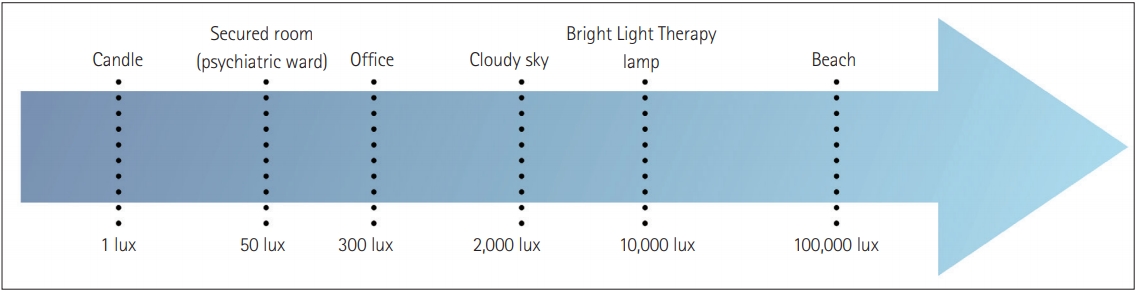
Following Rosenthal’s publications, the scientific community’s interest in light therapy became increasingly important. The devices used in Bright Light Therapy (BLT) are now a part of the personal care industry and are being miniaturized or portabilized; they should provide a light intensity going from 2000 to 10,000 lux [16]. Figure 4 displays two different examples of existing BLT devices including BLT glasses. As a comparison, a candle emits an intensity of about 1 lux, an office is estimated at 300 lux; outdoors, on a cloudy day in an urban area, light intensity is estimated to be 2,000 lux, but on a sunny day on a beach, this intensity is close to 100,000 lux. The light intensity of an intensive care room in a psychiatric ward would be about 50 lux. Figure 5 summarizes the different intensities of light across these conditions.
The 2000s witnessed the emergence of personal light lamps, getting more and more manageable, and new devices such as dawn simulators or portable light therapy glasses.
A large number of studies have since been carried out, initially about SAD, then about non-seasonal major depressive disorder (MDD) [17]. More recent studies are now focusing on the use of new BLT devices in seasonal and non-seasonal bipolar depression [18-20]. The evolution of light therapy from heliotherapy to BLT is summarized in Figure 6.
APPLICATION TO MOOD DISORDERS AND PHYSIOLOGICAL INSIGHTS
In order to be defined as BLT devices, the luminous intensity delivered must be higher or equal to 2,500 lux [16]. Most of the lamps emit an intensity of 10,000 lux, making it possible to decrease the duration of exposure.
Regarding the seasonal affective disorder
The BLT is now recognized as the first-line treatment of depressive episodes in SAD. Its use is recommended as soon as the photoperiod decreases. The use of the Morningness-Eveningness Questionnaire has made it possible to create an algorithm for the use of BLT in this condition [21]. The BLT must be applied in the morning upon awakening, with an intensity of 10,000 lux for 30 minutes, daily; or 5,000 lux for 1 hour and 2,500 lux for 2 hours [16].
Bright light therapy for major depressive disorder
The use of BLT in MDD is now recommended as an adjunctive therapy to conventional antidepressants (for example fluoxetine, sertraline and imipramine) [17,22-26]. The recommended dosage is equivalent to that of the SAD depressive episode. Other research focuses on possible therapeutic associations of BLT with agomelatine, melatonin, wake therapy and sleep deprivation [17,22-26].
Bright light therapy for bipolar disorder
The use of BLT during depressive episodes in patients with bipolar disorder should consider the risk of manic shift and should be done in the presence of an effective mood stabilizing treatment [16,27]. There is currently no existing proper and validated algorithm like there is in unipolar disorders, but current studies could help to establish guidelines to maximize the antidepressant effects of BLT while limiting the risk of manic or hypomanic shift [28]. The treatment should follow a slow increase in duration, and may start at 7.5 minutes per day, upon waking, to be gradually increased (weekly) to 15 minutes then 30 minutes per day [28]. An intensity of 10,000 lux (or equivalent) may be used, but can be decreased for tolerance or comfort issues, keeping in mind that a proportional increase of the duration should be proposed (as in the SAD paragraph).
There is currently no consensus regarding BLT in bipolar depression, but we recommend using this treatment under close medical supervision, so that the duration of exposure can be adjusted rapidly if the patients were to show hypomanic symptoms such as irritability, psychomotor agitation, or sleep disorders. In case of poor tolerance, the duration of exposure should be reduced and the time of exposure may be shifted to midday, as suggested by the study from Sit et al. [27] and by Chronotherapeutics for Affective Disorders: A Clinician’s Manual for Light and Wake Therapy [21].
Physiological insights
The light coming to the eye sends to the brain two different types of information: the so-called “visual” information, relayed by photoreceptors known as rods and cones; whereas “non-visual” information results from the detection by the eye of variation in light intensity and is then transmitted to the brain through melanopsin. This photosensitive protein discovered in the early 2000s and its major role in mediating the effects of light has been the subject of numerous research [29].
In the SAD, it is the action of light on the indirect circadian process that seems to be at the origin of the therapeutic efficacy of BLT on mood disorders, this mechanism would be influenced by external light information, thus influencing the production of melatonin by the pineal gland in the brain [13] via Supra-Chiasmatic Nuclei (SCN) or central biological clock. The mechanism involved in the non-seasonal depressive disorder would be the indirect effect of melanopsin. Expressed by intrinsically photosensitive Retinal Ganglion Cells (ipRGCs), its production is strongly stimulated by blue light [30]. The role of melanopsin is therefore to transmit information concerning light intensity to structures strongly involved in the regulation of sleep, arousal and circadian rhythms, more precisely the SCN and the ventrolateral preoptic nuclei. As shown by research involving genetic manipulation, mice deprived of ipRGCs would tend to get depressed and lose weight [31].
Even more recent studies observe that light may exert a direct action (non-circadian action) on monoaminergic systems [32], and as such directly associate the influence of light on the endogenous production of Serotonin (5-HT). BLT and serotoninergic drugs would exert synergistic antidepressant effects in the polymorphism of the 5-HT transporter. This would confirm the hypothesis that BLT shares the neurobiological mechanisms of action of serotonergic drugs. Indeed, the BLT tends to increase the levels of tetra-hydro-biopterin, essential cofactor of the hydroxylation of tryptophan and itself essential to the synthesis of 5-HT [33]. In line with this, some light-therapy lamps use a blue-enriched light (λ=468 nm), attributed to a maximal antidepressant effect by its action on melanopsin and monoamines including 5-HT.
The anti-depressive action of the BLT would therefore be the sum of two interconnected processes—direct and indirect—mediated by the RGCs and the ipRGCs.
DISCUSSION
BLT has a rapid action on depressive symptoms with observable results from the first days of treatment, although some studies have periods of exposure of up to 6 weeks [34] or even 8 weeks for the SAD, this extended exposure would not show any additional efficacy [35]. All these results are consistent with the literature regarding the efficacy of BLT in bipolar depression, which can be as high as 78% in some trials [18,20]; as well as seasonal bipolar depression [29].
Regarding the tolerance of BLT in BD, the data in the literature are more contradictory [36] with debates still very recent in the American Journal of Psychiatry [37,38]. Unfortunately, there is mainly a lack of reliable data (only 2 studies used standardized scales for manic symptoms, the YMRS), and the vast majority of available studies included unipolar and bipolar patients. The randomized BLT trial (7,000 lux/day at mid-day) against placebo (dim red light therapy, dRLT) of Sit and colleagues [39] in which were included patients with BD with and without seasonal patterns reported no cases of manic or hypomanic shift despite a larger number of patients included (n=23 in each group), and observe that a mid-day exposure appeared safe in patients with BD. On the other hand, regarding morning exposure, the same safety observations were also made by the Zhou et al. [20] placebo-controlled trial including 74 patients (BLT=33 patients, dRLT=30 patients), and by the historical review of Benedetti [36], gathering forty-one studies of BLT in bipolar depression and concluded that there was a minimal risk of mood shift, regardless of treatment modalities (intensity, time of day, duration of exposure): only 0.9% for a manic episode, 1.4% for a hypomanic episode. Nevertheless, these data are not standardized and mix several populations of unipolar/bipolar, seasonal/non-seasonal patients. Also, only 13 studies of the 41 selected by Benedetti [36] used a light intensity of 10,000 lux/day. As a result, those results cannot be generalized to the main population. Finally, particular precautions for the use of BLT in BD would also apply to rapid cycling patients, where the rate of switch would be of 18.8% [27].
CONCLUSION
Heliotherapy has been the longest used form of phototherapy and the only one until the mid-nineteenth century. Since the invention of the electric light bulb and the progress of medicine, heliotherapy shifted to UV phototherapy and to light therapy (UV filtered light). BLT is today the gold standard treatment of the SAD, and is recommended in various others affective disorders with non-seasonal patterns. Recent findings helped to better understand the physiological insights underlying BLT’s action on affective disorders and may pave the way toward an optimal use in mood disorders.
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Jérémy Choukroun, Pierre Alexis Geoffroy. Data curation: Jérémy Choukroun, Pierre Alexis Geoffroy. Formal analysis: Jérémy Choukroun, Pierre Alexis Geoffroy. Funding acquisition: Jérémy Choukroun, Pierre Alexis Geoffroy. Investigation: Jérémy Choukroun, Pierre Alexis Geoffroy. Methodology: Pierre Alexis Geoffroy. Project administration: Pierre Alexis Geoffroy. Resources: Pierre Alexis Geoffroy. Software: Jérémy Choukroun, Pierre Alexis Geoffroy. Supervision: Pierre Alexis Geoffroy. Validation: Jérémy Choukroun, Pierre Alexis Geoffroy. Visualization: Jérémy Choukroun, Pierre Alexis Geoffroy. Writing—original draft: Jérémy Choukroun, Pierre Alexis Geoffroy. Writing—review & editing: Jérémy Choukroun, Pierre Alexis Geoffroy