Pharmacological Treatment for Rapid Eye Movement Sleep Behavior Disorder
Article information
Abstract
Rapid eye movement (REM) sleep behavior disorder (RBD) is a parasomnia characterized by abnormal movement during REM sleep. Violent motor behaviors correlated with dreams commonly result in sleep-related injuries, which are sometimes life-threatening, to patients and their bed partners. The current guidelines for RBD treatment include counseling, modifying the sleep environment to prevent sleep-related injury, and pharmacological therapy. This paper focuses on current pharmacotherapy options for the treatment of RBD, including clonazepam and melatonin, which represent the mainstay of RBD therapy. Acetylcholinesterase inhibitors and dopamine-agonists have been used, as RBD is usually associated with other neurodegenerative diseases, with encouraging results in preliminary clinical trials. More randomized controlled trials with objective outcome measures are needed to assess both short-term and long-term effects of these medications and their efficacy in RBD. Understanding the exact mechanisms involved in decreasing RBD symptoms could provide future approaches in new drug development.
INTRODUCTION
Rapid eye movement (REM) sleep behavior disorder (RBD) is a parasomnia characterized by abnormal movement during REM sleep [1]. This REM parasomnia disorder was first reported in 1986 by Schenck et al. [2], and has been referred to as RBD since 1987 [3]. RBD can occur alone as the idiopathic form or in association with other neurological diseases, in particular the α- synucleinopathies, including Parkinson’s disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA) [4]. In a longitudinal cohort study, the rate of phenoconversion to neurodegenerative disease was 10.6% after 2 years, 31.3% after 5 years, 51.4% after 8 years, and 73.5% after 12 years [5]. The median phenoconversion time was 8 years. Potential prodromal synucleinopathy signs include subtle motor, cognitive, olfactory, and autonomic abnormalities in patients with RBD [6].
RBD occurs in repeated episodes of dream-enacting behavior (DEB) such as punching, arm flailing, kicking, or sleepwalking, usually accompanied by vivid dreams during REM sleep. REM sleep without atonia (RSWA) is a key polysomnographic hallmark of RBD. Dysregulation within the brainstem regions involved in regulating REM-related muscle atonia is thought to be the basis of RSWA [7]. Patients and their bed partners frequently suffer sleep-related injuries, sometimes life-threatening, as a result of violent motor behaviors correlated with dreams [8]. The current guidelines for RBD treatment include modification of the sleep environment to reduce the risk of sleep-related injury and pharmacological treatment. This review provides an overview of the recent advances in RBD pharmacotherapy and recent research trends.
FIRST-LINE PHARMACOLOGIC TREATMENT OPTIONS FOR RBD
Clonazepam, a potent, long-acting benzodiazepine, has long been regarded as the first-line treatment for RBD. The exact therapeutic mechanisms of clonazepam in RBD are not fully understood, although it may reduce the frequency of unpleasant dreams, thus decreasing violent dream enactment behavior. An earlier study found that clonazepam selectively decreases REM sleep phasic activity but exerts no effect on REM sleep atonia [9]. Clonazepam improved dream content and reduced vigorous DEBs in a recent prospective observational study of 39 idiopathic REM sleep behavior disorder (iRBD) patients [10]. However, total and tonic electromyography activities during REM sleep significantly increased, despite improvements in clinical RBD symptoms. This is in line with the observations of Iranzo et al. [11]. These findings imply that clonazepam has a greater impact on dreaming and sleep quality than the pathophysiology of REM sleep atonia loss in RBD.
The existing data on the effects of clonazepam on the REM sleep parameters in RBD patients are inconsistent. Clonazepam has been the recommended treatment since the first clinical description of RBD by Schenck et al. in 1986 [2]. Indeed, the clinical efficacy rate was reportedly up to 90% in subsequent case series and open-label studies [12]. Olson et al. [13] reported 87% of RBD patients had a partial or complete response to clonazepam treatment.
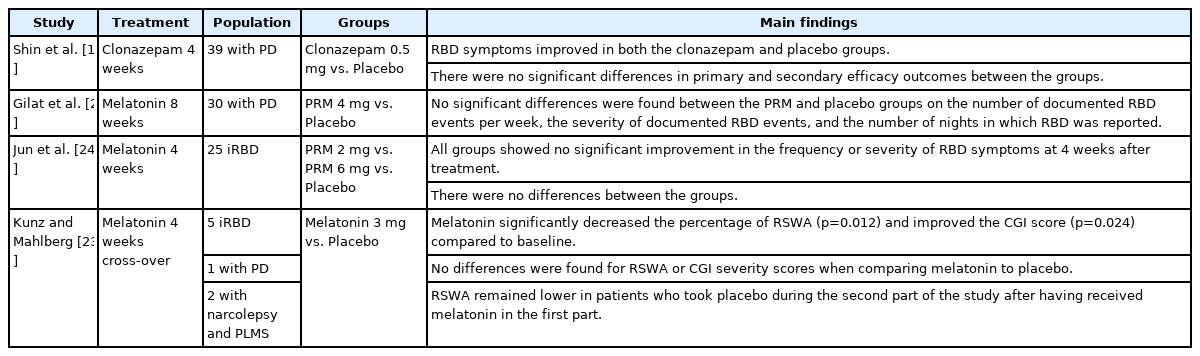
Long-term clonazepam administration did not reduce objective or subjective RBD severity in two retrospective studies by Ferri et al. [14,15]. Recently, a four-week, double-blind, randomized controlled trial (RCT) examined the effect of clonazepam on RBD in PD was reported [16]. Interestingly, RBD symptoms improved in both the clonazepam and placebo groups, but there was no significant difference between the two. Also, no improvements following clonazepam were noted on any of the secondary subjective sleep severity outcomes as compared to placebo (Table 1). In an electroencephalogram (EEG) study of clonazepam treatment in iRBD patients, <15 Hz EEG band suppression was reduced in drug-naïve iRBD patients, which was partially recovered after clonazepam treatment [17]. More studies are recommended to determine if there is an objective improvement of RBD with clonazepam compared with a placebo.
Only a limited amount of data is available regarding the effects of other benzodiazepines on RBD. A retrospective case series demonstrated temazepam and zopiclone improved RBD symptoms in iRBD patients over the age of 50 [18]. Another retrospective case series reported effective use of zopiclone as a combination therapy in an elderly RBD patient [19].
Melatonin, produced and secreted mainly in the pineal gland at night, plays an important role in regulating diverse circadian rhythms, including sleep. After Kunz and Bes [20] reported melatonin’s effects on a 64-year-old male patient with RBD in 1997, subsequent studies have reported its effects. An early small case series demonstrated that melatonin has an up to 90% efficacy in treating RBD. Takeuchi et al. [21] found that melatonin remarkably ameliorated RBD symptoms and tonic REM muscle activity in 13 of 15 patients. Melatonin treatment worked well in patients with low basic melatonin concentrations and demonstrated a dose-dependent effect. Boeve et al. [22] showed persistent benefit with melatonin (with or without concomitant low-dose clonazepam) beyond one year of therapy in 57% of patients.
A first cross-over RCT by Kunz and Mahlberg [23] compared the effects of four weeks of 3 mg melatonin to the effects of four weeks of 3 mg of matched placebo across all subjects. Patients were instructed to take melatonin between 22:00 and 23:00 and to go to bed within 30 minutes of melatonin administration. Melatonin significantly reduced the number of REM sleep epochs without muscle atonia and led to a significant improvement in clinical global impression. Interestingly, the number of REM sleep epochs without muscle atonia remained lower in patients who took the placebo during the second part of the study after having received melatonin at first. This suggests that the effects of melatonin could last even after stopping for several weeks. In a four-week, randomized, double-blind, placebo-controlled pilot study, Jun et al. [24] tested the effects of prolonged-release melatonin (PRM) on iRBD. Participants were randomly assigned to receive PRM 2 mg/day, PRM 6 mg/day, or placebo for four weeks. They found no significant improvement in all groups at four weeks, with no differences among the groups. In another RCT, Gilat et al. [25] compared the effects of PRM 4 mg to placebo 4 mg for eight weeks in 30 PD patients with RBD. There were no significant differences between the PRM and placebo groups on any of the RBD-related outcome measures, including the number of RBD events per week and the number of nights with REM sleep behavior (Table 1). As small RCTs may have limitations, including small sample size and a lack of objective outcome measures, the results cannot be generalized to all patients with RBD.
Given the proposed mechanism of action for melatonin in RBD, melatonin receptor antagonists could be potentially useful agents for RBD treatment. Ramelteon, a melatonin receptor agonist, improved RBD symptoms and decreased RSWA in two patients with RBD secondary to MSA and PD when given at a dose of 8 mg/day [26]. In a pilot open-label treatment trial of ramelteon in iRBD patients, Esaki et al. [27] found that 7 of 10 patients had improved subjective DEB frequency and severity despite inadequate response on objective polysomnographic RBD behaviors or RSWA. In a case series of three patients, 25–50 mg agomelatine, a melatonin 1 and 2 receptor agonist, before bedtime reduced the frequency and severity of RBD episodes without affecting REM muscle tone [28].
Melatonin’s mechanism of action against RBD remains unclear, but it may exerts its therapeutic effect by reducing tonic REM activity and restoring circadian rhythm desynchronization [21]. Clonazepam exerts its effect by suppressing violent DEBs and reducing excessive phasic muscle activity. Therefore, melatonin can be useful as an additive therapy due to its complementary activity.
ALTERNATIVE TREATMENTS FOR RBD
Acetylcholine (ACh) plays an important role in regulating REM sleep. Muscle atonia during REM sleep may be regulated by the pedunculopontine/laterodorsal tegmental nucleus, which contains cholinergic neurons that are active during REM sleep [29]. Cholinergic agonists into the brainstem produce REM sleep and REM sleep muscle atonia, whereas cholinergic antagonists inhibit these effects [30]. Therefore, administration of an Acetylcholinesterase inhibitor (AChEI) could increase ACh in the brain and reactivate physiological atonia during REM sleep. Di Giacopo et al. [31] tested rivastigmine in 12 RBD patients with PD who were resistant to conventional first-line treatments (melatonin and clonazepam). The rivastigmine treatment group showed a significant reduction of RBD episodes. In another placebo-controlled, crossover pilot trial involving a cohort of 25 patients with mild cognitive disorder, rivastigmine significantly improved RBD symptoms [32]. Ringman and Simmons [33] reported marked improvement of RBD symptoms with another AChEI, donepezil, in three patients. A 24-week, double-blinded RCT demonstrated the efficacy of memantine, a competitive N-methyl-D-aspartate receptor antagonist, on RBD symptoms in patients with DLB and PD [34]. On the other hand, AChEIs was reported to induce RBD in the patients with Alzheimer’s disease [35]. The effect of AChEIs on RBD symptoms is still controversial. It will be necessary to evaluate the effectiveness of AChEIs and neuroprotective agents in iRBD, not associated to cognitive impairment.
The high prevalence of RBD in PD and periodic limb movement disorders related to dopamine deficiency supports the hypothesis that RBD is caused by an abnormality in the nigrostriatal dopaminergic system. Reduced striatal dopamine innervation in iRBD patients was reported in a PET imaging study [36]. Pathological substantia nigra hyperecogenity was observed in both iRBD and PD patients [37]. Several open-label studies on dopamine-agonists (pramipexole, ropinirole, and rotigotine) have demonstrated effectiveness on RBD symptoms [38-40]. However, Kumru et al. [41] showed pramipexole improved parkinsonism but did not change RBD symptoms in PD patients. In a retrospective study conducted on 250 patients with PD, levodopa daily dose was significantly associated with RBD symptom severity [42]. Therefore, the effects of dopaminergic treatment on RBD symptoms remain controversial.
Sodium oxybate (SO) has been reported as one of the effective monotherapy or adjunct therapy for RBD [43-45]. SO is a drug for treating cataplexy and somnolence in narcolepsy. SO may mediate its effects through GABA-B receptors. Administration of 3 g to 6 g of SO was effective in RBD comorbid with narcolepsy type 1 and also in RBD treatment-resistant cases. SO might be an alternative treatment option for patients not responsive to other conventional treatment options, such as clonazepam and melatonin.
CONCLUSION
Although several clinical observations and case series have demonstrated the efficacy of clonazepam and melatonin, existing evidence is lacking. Some alternative agents might be useful for patients with RBD who are resistant to first-line treatment. AChEIs and dopamine-agonists might be a good treatment option for patients with other neurodegenerative diseases. More RCTs with objective outcome measures are needed to assess both short- and long-term effects of these medications and their efficacy in RBD. Understanding the exact mechanisms involved in decreasing RBD symptoms could promote new drug development.
Acknowledgements
This study was supported by National Research Fund (NRF2020R1A2C1008072), Republic of Korea. The funder had no role in the design and conduct of the study, and in the decision to submit the article for publication.
Notes
The author has no potential conflicts of interest to disclose.