Eveningness and Impulsivity in Euthymic Mood States Adversely Affect the Quality of Life of Major Depression and Bipolar Disorder Patients
Article information
Abstract
Objective
Chronotype and impulsivity are important features to be examined in mood disorder patients; these characteristics precede mood disorder onset and persist between mood episodes. Moreover, quality of life is an important outcome in psychiatric patients. This study investigated the interaction between these features and its effect on mood disorder patient’s quality of life.
Methods
Early-onset major depressive disorder (MDD), bipolar disorder I (BD I), and bipolar disorder II (BD II) patients were recruited. Excluding 18 patients who were missing data on main variables and 5 patients who were classified as severely ill, a total of 472 euthymic patients (MDD=167, BD I=133, BD II= 172) were assessed on their chronotype, trait impulsivity, and quality of life using self-reports.
Results
Both impulsivity and eveningness were negatively associated with quality of life. Regression results showed that there was a significant interaction effect between eveningness and impulsivity on quality of life. This indicates that the higher the level of impulsivity in mood disorder patients, the negative effect of eveningness on quality of life increased.
Conclusion
The current study suggests that examination of impulsive personality in relation to chronotype may be important in further understanding the effects of these features on mood disorder patients’ lives.
INTRODUCTION
Chronotype is a clarification of one’s preferences for activity and sleep [1]. Morningness is placed at one end of the continuum and eveningness at the other end. Individuals have different preferences in chronotype; people who are morning-oriented tend to sleep and wake up earlier and engage in morning activities than evening-oriented people do [2].
Previous research on chronotype has found correlations with mental health. Evening-oriented individuals are more vulnerable to mood episodes than those who are more morning-oriented [3]. Studies have reported that evening preference was more prevalent in patients with major depressive disorder or symptoms [4-8] and bipolar I and II disorders [9-12] than in healthy individuals. On the other hand, morningness is known to be associated with life satisfaction [13].
Chronotype has also been found to be associated with different personality dimensions. Several studies have reported the association between eveningness and impulsivity [14]. Impulsivity is a personality trait that has been studied relatively thoroughly in psychiatric population, especially in mood disorders [15]. Specifically, heightened impulsivity is a key feature of bipolar disorders [16].
Eveningness and impulsivity persist across depressive and (hypo) manic states in mood disorder patients [17]. Although studies thus far have reported that eveningness and impulsive trait as potential risk factors for mood disorders, there are few studies that simultaneously investigated the interaction between these two key features in a large cohort of mood disorder patients. Thus, investigating how mood disorder patients’ diurnal preference and trait impulsivity interactively affect their lives may clarify more about potential risks for mood disorders.
Self-reported chronotype and impulsivity were predictor variables. Self-reported quality of life was the outcome variable. Good quality of life implies more than just good health. It is an essential indicator of well-being [18]. Michalak et al. [18] suggest that the assessment of quality of life in psychiatric patients is valuable because it measures how patients live and more about the patients not just the symptoms nor the outcome of treatments. The goal of this study was to examine the relationship between chronotype, impulsivity, and quality of life in early-onset mood disorder patients. We hypothesized that 1) eveningness is negatively correlated with quality of life, 2) impulsivity is also negatively correlated with quality of life, and 3) higher the level of impulsivity, the negative effect of eveningness on quality-of-life increases.
METHODS
Participants
A total of 495 participants were initially recruited as part of the Mood Disorder Cohort Research Consortium (MDCRC) study. The MDCRC study is a multicenter prospective observational cohort study on early-onset mood disorders in South Korea (ClinicalTrials.gov: NCT03088657). The inclusion criteria for the participants were: 1) diagnosis of major depression disorders (MDD), bipolar disorder I (BD I), or bipolar disorder II (BD II), 2) younger than 25 years or less than 2 years of treatment duration. Details were described in Cho et al. [19]. Data were collected at nine different sites: Korea University Anam Hospital, Seoul National University Hospital, Seoul National University Bundang Hospital, Samsung Medical Center, Severance Hospital, Pusan National University Hospital, Gyeongsang National University Hospital, Cheonnam National University Hospital, and the National Center for Mental Health. Participants were diagnosed with the Mini-International Neuropsychiatric Interview [20]. Informed consent was obtained from all participants prior to the study, and this study was reviewed by the Institutional Review Boards for all nine participating hospitals (2015AN0239).
A total of 23 participants were excluded. First, 18 participants were excluded due to missing data on main variables. Additional 5 participants were excluded from the sample due to symptom severity; participants who scored greater than 35 on Korean Montgomery–Asberg Depression Rating Scale and 25 on Young Mania Rating Scale were classified as severely ill and thus could not be reliable due to the mood symptoms [21,22]. A total of 472 patients, who were relatively euthymic (167 MDD patients, 133 BD I patients, and 172 BD II patients) were selected for analysis.
Measures
Impulsivity
Barratt impulsiveness scale (BIS) developed by Barratt et al. [23] and later validated in Korean by Lee et al. [24] was employed to assess impulsivity. The questionnaire is of 30 items on a 4-Likert scale. Higher scores indicate a higher level of impulsivity. The Korean version of the BIS is found to be reliable and valid [24].
Quality of life
The World Health Organization Quality of life Scale Abbreviated version (WHOQOL-BREF) developed by The WHO group [25] and validated in Korean by Min et al. [26] was used to examine quality of life. The questionnaire is of 26 items on a 5-Likert scale. Higher scores indicate higher quality of life. The Korean version of WHOQOL-BREF showed adequate validity and reliability.
Statistical analyses
First, we conducted Pearson’s correlation tests to examine the relationship between the three main variables. Then, linear regressions were conducted to examine the effect of eveningness, impulsivity, and their interaction on quality of life. We also performed hierarchical regression to assess whether the regression model including the interaction explains larger variance of quality of life than the original model does. Data analyses were conducted using the R program (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
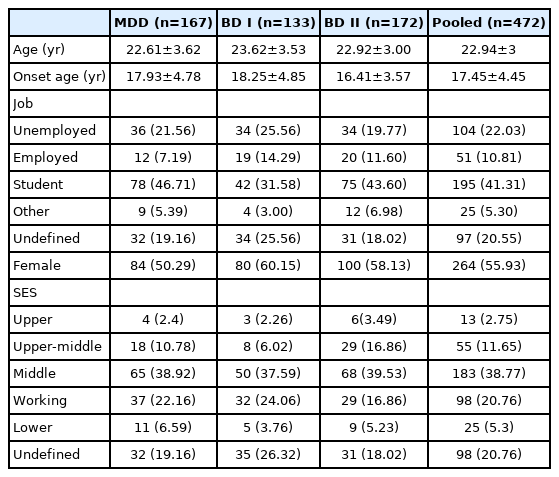
Table 1 shows the sociodemographic characteristics of participants with MDD, BD I, BD II, and pooled population.
Association between chronotype, impulsivity, and quality of life
First, we conducted Pearson’s correlation tests to examine the relationship between the three main variables: eveningness, impulsivity, and quality of life. First, impulsivity was negatively correlated with quality of life (r=-0.23, p<0.001). Also, impulsivity was positively correlated with eveningness (r=0.26, p<0.001). Moreover, eveningness was negatively correlated with quality of life (r=-0.35, p<0.001).
We then conducted hierarchical regressions to examine the interaction effect between impulsivity and eveningness on quality of life (Table 2). The result showed a significant effect of eveningness on quality of life, β=-0.29, p<0.001, 95% CI [-0.37, -0.21]. That is, participants who were more evening-oriented reported lower quality of life. This effect of eveningness on quality of life was qualified by the level of impulsivity β=0.11, p=0.004, 95% CI [0.04, 0.19]. Specifically, the higher the level of impulsivity, the negative effect of eveningness on quality of life increased.
The model including the interaction between impulsivity and morningness (Model 2) explained larger variance of quality of life than did the model only including the main effect (Model 1) (F=8.49, p=0.004). Moreover, the results remained significant even after controlling for the effect of sociodemographic variables including sex, age, socioeconomic status, age of onset, and job classification β= 0.13, p=0.003, 95% CI [0.05, 0.22].
DISCUSSION
The aim of the current research was to examine the relationship between chronotype, impulsivity, and quality of life in a multicenter cohort study on mood disorders. First, our results indicated that there was a negative correlation between impulsivity and quality of life. Also, eveningness was negatively correlated with quality of life. Most importantly, there was an interaction effect between eveningness and impulsivity on quality of life. That is, for mood disorder patients who are more impulsive, the negative effect of eveningness on quality of life increased. This interaction effect remained significant even after controlling for sociodemographic variables. Finally, the model including the interaction between eveningness and impulsivity explained a larger variance of quality of life than did the one that only included the main effect. Our results are consistent with those of previous studies that indicated associations between chronotype, impulsivity, and quality of life in mood disorder patients.
Previous studies have reprorted that chronotype [29] and impulsivity [30] are associated with mood disorders. Specifically, eveningness and heightened impulsivity have been identified as risk factors for mood disorder patients. Although there are many studies that showed that evening chronotype and heightened impulsivity as contributors to risk for mood psychopathology, relatively limited literature has focused on the interactive effect of these features. On top of the well investigated positive association between eveningness and impulsivity [31], the current findings suggest that those who were more evening-oriented with higher trait impulsivity reported lower quality of life. This is in line with recent literature that mood disorder patients who were more impulsive when slept later showed more mood symptoms the next day [32].
The current study has several limitations. First, this study was a cross-sectional and descriptive study. Future longitudinal study should assess how changes, either increase or decrease, in the level of impulsivity interact with chronotype to affect quality of life. Also, despite the nuanced information delivered by examining quality of life in mood disorder patients, future studies may assess mood symptoms, episode recurrences, which would provide more clinically significant outcomes. Moreover, although we chose to examine patient’s preference in activity and sleep, it may be important to objectively measure sleep disruption and misalignment.
Despite the limitation, this study contributes to the knowledge about the relationship between chronotype and impulsivity and how they affect mood disorder patients’ lives. This suggests that examining the impulsive personality trait in relation to diurnal preference may be helpful in understanding further about the outcomes of quality of life in patients with mood disorders.
Notes
Funding Statement
HJL is supported by grant number HM14C2606 from the Ministry of Health & Welfare and grant number 2017M3A9F1031220/ 2019R1A2C2084158 from the National Research Foundation of Korea.
The authors have no potential conflicts of interest to disclose.
Availability of Data and Material
Deidentified participant data that underlie the results reported in this article can be shared with investigators for research purposes. To gain access, data requests can be made by contacting the corresponding author, HJL.
Author Contributions
Conceptualization: Heon-Jeong Lee. Data curation: Sojeong Kim, Yeaseul Yoon. Formal analysis: Sojeong Kim, Yeaseul Yoon. Investigation: Sojeong Kim, Yeaseul Yoon. Methodology: Sojeong Kim, Yeaseul Yoon. Resources: Sojeong Kim, Yeaseul. Software: Sojeong Kim. Supervision: Heon-Jeong Lee. Validation: Sojeong Kim, Yeaseul Yoon. Visualization: Yeaseul Yoon. Writing—original draft: Sojeong Kim, Yeaseul Yoon. Writing—review & editing: Heon-Jeong Lee.