Sleep Duration and Body Mass Index in 5–9 Aged Korean Children
Article information
Abstract
Objective
Since sleep duration has been suggested to play an important role in the development of obesity in children, the risk factors for insufficient sleep have received increasing attention. The aim of this study was to investigate the sleep duration and compare it with obesity with sleep duration in children aged 5–9 years.
Methods
This cross-sectional study was conducted using Dietary Screening Test which is a parent-reported questionnaire administered to Korean children aged 5–9 years between January 2021 and July 2022. Data including sleep duration and bedtime were obtained. Body mass index (BMI) was categorized into the following four groups according to the age-specific BMI criteria: underweight, normal weight, overweight, and obesity.
Results
Altogether, 15,543 out of the 22,055 participants, comprising 7,605 (48.9%) boys and 7,938 (51.1%) girls aged 5–9 years, were finally included in the analysis. The proportion of participants above the 85th percentile was 24.3%. The average sleep duration was 9.40±0.88 h. A comparison of sleep duration between the four BMI groups showed a significant difference in sleep duration at 5, 6, and 7 years of age (p<0.05). The bedtime for children aged 5 to 9 years was 21.69±0.75 h. There was a significant difference in bedtime at 9 years of age among the four BMI groups (p<0.05).
Conclusion
In this study of Korean children, the obesity group had the shortest sleep duration at the age of 5–7 years and latest bedtime at age 9. These results may contribute to a better understanding of interventions to achieve sufficient sleep duration and prevent obesity in children.
INTRODUCTION
Sufficient sleep is important for the growth, maturation, and health of children and adolescents [1]. Sleep deprivation during childhood may interfere with physiological restoration, leading to biological and behavioral problems and chronic disease development, including obesity, depression, and cardiovascular disease [2-4]. It is also reported to be associated with impairment in concentration, hyperactivity, and poor academic performance [5,6]. Nowadays, children are not getting enough sleep, and their sleep duration has decreased. A study in the United States reported a secular decline of 0.75 minutes/year in children’s sleep duration over the last 100 years [7].
Conversely, the prevalence of pediatric obesity has increased over the past few decades worldwide, including obesity in preschool-aged children, which has become a serious public health concern [8]. Children with obesity have a high probability of becoming obese in adulthood, with higher risks of developing hypertension, diabetes, respiratory problems, certain cancers, and other chronic diseases [2,3,9], which significantly overlaps with those caused by insufficient sleep.
The identification of modifiable factors associated with obesity is important for preventing and managing obesity in children. Many studies have found an inverse linear correlation between sleep duration and obesity in older children and adolescents [10-12]. Moreover, a longitudinal study reported that a sleep duration of <12 h in infancy was associated with being overweight in children at 3 years of age [11]. Earlier bedtimes at preschool age were associated with a lower risk for adolescent obesity [13].
Since sleep duration has been found to play an important role in the development of obesity in both children and adolescents, there is a growing need to investigate the mechanisms of sleep duration and obesity. The mechanism by which sleep deprivation may affect obesity has not been well explained, but several possibilities have been suggested, which are as follows [14]: 1) increased free time increases food intake; 2) sleep deprivation affects hormone secretion, including decreased leptin and elevated ghrelin levels as well as increased insulin insensitivity [15,16]; and 3) tiredness due to sleep deprivation could lead to a decrease in physical activity and a consequent reduction in energy expenditure [17].
The association between short sleep duration and obesity emphasizes the importance of sleep duration in preventing obesity in childhood. However, many studies have focused on older children and adolescents, whereas studies on obesity in young children are limited. The aim of the present study was to investigate the sleep duration and association of obesity with sleep duration in children aged 5–9 years.
METHODS
This cross-sectional study was performed using Dietary Screening Test which is a parent-reported questionnaire administered to Korean children aged 5–9 years between January 2021 and July 2022. This survey was conducted in cooperation with public health centers, the Children’s Food Center Management Support Center, etc., through an online survey platform (Nutri-I Eye Care Solution, 2016) developed by the Nutrii Life Cycle Food Research Institute (Seoul, Korea).
Data on sex, age, height, weight, sleep duration, time to sleep, underlying disease, and drug use of the child were obtained using the questionnaire. Sleep duration data were acquired using the following question in the self-reported questionnaire: “How many hours does your child sleep on average?”
Body mass index (BMI) was calculated by dividing body weight (kg) by height squared (m2). BMI was categorized into the following four groups according to age-specific BMI criteria by the Korean Centers for Disease Control and Prevention, which used physical growth measurement surveys conducted in 1997 and 2005 [18]: underweight (BMI <5th percentile), normal weight (BMI between the 5th and 84th percentiles), overweight (BMI between the 85th and 94th percentiles), and obese (BMI ≥95th percentile).
Statistical analysis
Statistical analysis was performed using the R statistical programming language, version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria). We used an analysis of variance test to compare the sleep duration between BMI groups, followed by Tukey’s post hoc analyses. Values are presented as mean± standard deviation for descriptive statistics. Time is presented as military time and converted to hours for statistical analysis.
Informed consent was obtained from the study participants. This study was approved by the Korea University Ansan Hospital Institute Review Board (IRB number: 2022AS0237).
RESULTS
Participants’ characteristics
Altogether, 15,543 out of 22,055 participants, comprising 7,605 (48.9%) boys and 7,938 (51.1%) girls aged 5–9 years, were finally included in the analysis. We excluded children with allergic diseases, congenital anomalies, and neurological diseases, and those taking a medication that can affect sleep.
The participants’ mean age was 74.7±13.4 months. Regarding BMI, the average BMI was 16.6±2.6 kg/m2, and 24.3% participants were above the 85th percentile (overweight group, 10.0%; obesity group, 14.3%) (Table 1).
Sleep duration and BMI
The average sleep duration for children aged 5–9 years was 9.40±0.88 h. Sleep duration decreases with increasing age, showing no significant differences between the sexes (p<0.05). Table 2 shows the sleep duration by age.
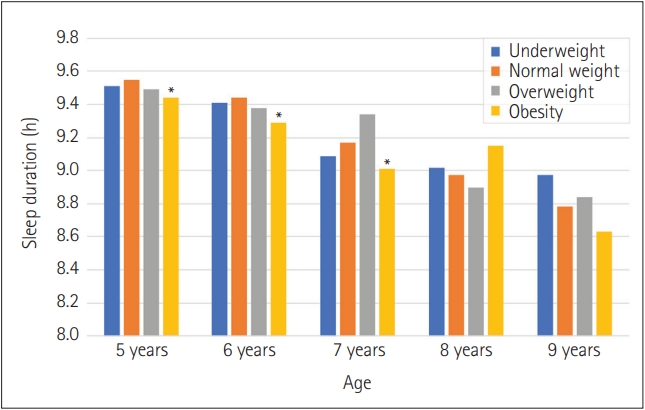
The comparison of sleep duration among the underweight, normal weight, overweight, and obesity groups showed significant differences in sleep duration at 5, 6, and 7 years of age (p<0.05) (Figure 1).
Bedtime and BMI
The bedtime for children aged 5–9 years was 21.69±0.75 h and they fell asleep later with increasing age.
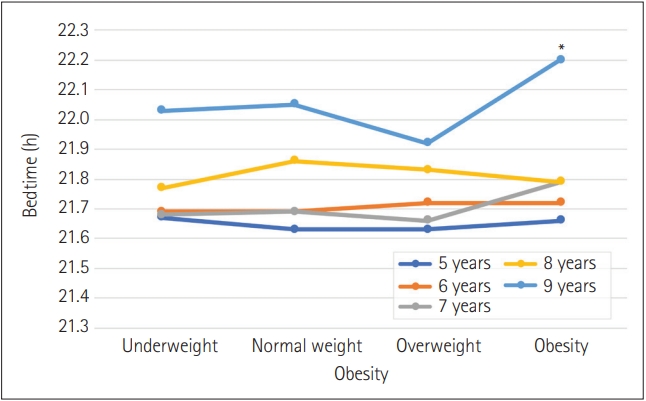
In the comparison of bedtimes among the underweight, normal weight, overweight, and obesity groups, there was a significant difference in the bedtimes in children at 9 years of age (p<0.05) (Figure 2).
DISCUSSION
In this study involving Korean children aged 5–9 years, the mean sleep duration was 9.40 h. The obesity group had the shortest sleep duration at the age of 5–7 years and the latest bedtime at the age of 9 years. To the best of our knowledge, this study is the first to investigate the association between sleep duration and obesity based on BMI in Korean children aged 5–9 years.
Sleep quality in children varies with age. Physiologically, the younger the age, the longer the sleep need. Children aged 3–5 years need at least 12 h of sleep, and school-age children aged 5–10 years need at least 10 h of sleep [1]. For older children and adolescents, 9–11 h and 8–10 h of sleep per night are recommended for 10–13- and 14–17-year-old children, respectively [19].
In this study, a mean sleep duration of children aged 5–9 years was reported to be <10 h, indicating that most Korean children, even those aged 5–6 years, did not have sufficient sleep duration. Compared to the results of studies in other countries, the sleep duration in our study was shorter. In England, a mean 11.5 h of sleep duration was reported in children aged 5–9 years [20]. German children had a mean sleep duration ranging from 10.89 h at 5 years of age to 9.76 h at 9 years of age [21]. Among the older children in Australia, 10.2 h of sleep a day was reported in those aged 9–11years [22].
A previous study of Korean infants and toddlers showed the latest bedtimes, shortest total sleep and daytime sleep durations, and least frequent rates of napping compared to other Asian and Caucasian children [23-25]. Infant and toddlers in Korea had a mean sleep duration of 11.89 h, which is relatively shorter than those of other Asian (12.33 h) and Caucasian children (13.02 h) [24]. Korean children aged 3–6 years had a mean sleep duration of 9.69 h, which is shorter than those of Canadian and Australian children (>10 h) [25]. These results, including those of our study, suggest that an inadequate sleep duration in Korean children begins from infancy and continues to early childhood. In a previous study conducted in Dunedin, which had the longest follow-up period, each additional hour of sleep in children aged 5–11 years predicted a mean BMI of approximately 1 unit lower at 32 years of age and approximately a 30% reduction in the risk of obesity (BMI ≥30 kg/m2) [26].
Late or irregular bedtimes may also affect the sleep duration and contribute to sleep problems, including behavioral difficulties. In addition, sleep timing and time to sleep might also be associated with obesity in childhood. Late bedtimes cause a decrease in the overall sleep duration. In this study, the participants’ mean bedtime was after 21:30. The 9-year-old children in our study went to bed after 22:00, which is a late bedtime comparable to those in other countries. In a large study involving 3–7-year-old children in England, children with non-regular bedtimes had more behavioral difficulties, and regular and earlier bedtimes were associated with fewer parent- and teacher-reported behavioral difficulties [27]. In a study involving 12-year-old children, children with obesity showed significantly later mean mid-sleep duration than children with normal weight [28]. Similarly, a prospective cohort of infants born in Japan in 2001 found that irregular and late bedtimes at 2 years of age predicted problems with behavior in the domains of attention and aggression at 8 years of age [29].
Sleep in young children is greatly influenced by several factors, such as cultural background and parents’ perception of sleep [25]. In Asia, including Korea, room sharing and bed-sharing are more common than in the West [23]. Compared to room sharing and sleeping alone, bed-sharing is known to be correlated with later bedtimes, later awakening times, and shorter duration of sleep [30]. Ahn et al. [24] reported that 94.5% of infants and toddlers in Korea slept in their parents’ rooms or beds. In Western countries, most sleep education emphasizes on the hazards of bed-sharing, such as impeding the development of autonomy and independence, fostering dependence on parents, and increasing the risk of sleep problems. In a study on bed-sharing in Korean children, for example, Yang and Hahn [31] found that 73.5% of mothers approved of bed-sharing in children between 3 and 6 years of age. The main reasons for bed-sharing were “to look after the child while sleeping” and “child too young to sleep alone.”
In addition, an increase in screen time and decrease in outdoor play might also be an issue. In children aged 2–5 years, screen time was associated with sleep duration, with more screen time being associated with less nocturnal sleep duration, prolonged sleep latency, and delayed bedtime [32].
Although a short sleep duration in adolescence has been attributed to delay in the circadian phases, attenuation of the build-up of sleep pressure [33] and the influence of external environmental factors, such as the use of electronic devices and social networking, are also significant, as compared to young children [34]. A study in Canada showed that a shorter sleep duration was associated with low family income with less educated parents and those with more screen time tended to have a shorter sleep duration [35]. However, in our previous study of South Korean adolescents, we found an inverse association between sleep duration and family income, contrary to that observed in a Western study [36]. These cultural and social factors can be improved through interventions and sleep education programs for parents or teachers.
Sleep at a young age has a greater impact on later obesity status. A recent meta-analysis reported that the association between short sleep duration and obesity was stronger in children aged 6–13 years than in those aged 1–2 and 14–17 years [37]. In a longitudinal study on sleep of children aged 3–5 years, later childhood obesity status of infants with sleep duration of <12 h a day was associated with a higher BMI z-score, higher sum of subscapular and triceps skinfold thickness, and increased odds of being overweight [11].
In addition, a meta-analysis by Chen et al. [38] reported a linear dose–response association in children aged <10 years; however, studies involving adolescents have inconsistent results. In an 8-year prospective cohort study, shorter sleep duration was more strongly associated with a higher BMI in middle childhood than in adolescence [39]. Therefore, ensuring a sufficient sleep duration in young children is important to prevent obesity.
Sleep recommendations for children play an important role in establishing public health policies and informing parents and children of healthy sleep behaviors. Many studies have reported that sleep management, including sleep education and cognitive–behavioral interventions, improves sleep-related habits, sleep quality, and academic performance [40-42]. In addition, research on children’s sleep duration is important so that parents are aware that their children do not get enough sleep. Therefore, an intervention program for sleep duration for children should be considered.
This study has a few limitations. First, sleep duration in this study was reported by parents without objective measures. This study was dependent on self-reported sleep durations. Moreover, there was no distinction between the weekends and weekdays. Despite these limitations, it is difficult to find a study on the sleep duration of Korean children aged 5–9 years with a large sample size.
In conclusion, our findings showed that young Korean children aged 5–9 years had short sleep durations and late betimes. These results may contribute to a better understanding of interventions to achieve sufficient sleep duration and to prevent obesity in children.
Notes
Funding Statement
This research was supported by a grant of the Korea Health Promotion R&D Project, funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HS22C0036). Also, this study was financially supported by Hansung University for Byoung Gook Loh.
The authors have no potential conflicts of interest to disclose.
Availability of Data and Material
The datasets generated or analyzed during the study are not publicly available due to proprietary right of Nutrii Co., Ltd. but are available from the corresponding author on reasonable request.
Author Contributions
Conceptualizations: Won Hee Seo. Data curations: Youngshin Han. Formal analysis: Wan II Cho. Methodology: Youngshin Han, Byoung Gook Loh. Writing—original draft preparation: Sung Hoon Yoo, Won Hee Seo. Writing—review and editing: Byoung Gook Loh.
Acknowledgements
None